doi: 10.62486/agmu202420
ORIGINAL
Frequency of community-acquired pneumonia in children aged 5 to 12 years in the Provincial Health Center N°48 of the city of Rosario
Frecuencia de Neumonía de la comunidad en niños de 5 a 12 años en el Centro de Salud Provincial N°48 de la ciudad de Rosario
Julieta Ivana Passas1
1Universidad Abierta Interamericana, Sede Rosario – Santa Fe. Argentina.
Cite as: Passas JI. Frequency of community-acquired pneumonia in children aged 5 to 12 years in the Provincial Health Center N°48 of the city of Rosario. Multidisciplinar (Montevideo). 2024; 2:20. https://doi.org/10.62486/agmu202420
Submitted: 05-12-2023 Revised: 19-04-2024 Accepted: 10-11-2024 Published: 11-11-2024
Editor: Telmo
Raúl Aveiro-Róbalo ![]()
ABSTRACT
Community-acquired pneumonia (CAP) is a relevant cause of morbidity in children under 10 years of age. This study at the Provincial Health Center N°48 in Rosario, Argentina, analyzed the frequency of CAP in children aged 5 to 12 years during 2023, using medical records of 30 patients. Fifty-three percent were girls and 47 % boys, with an average age of 8,37 years. The main risk factors were asthma, bronchial hyperresponsiveness and recurrent respiratory infections (40 %), malnutrition (33 %) and preterm birth (20 %). Common symptoms included fever, productive cough and chills. Ninety percent of the cases were treated with oral Amoxicillin. It is concluded that the frequency of CAP was low (4 %) and that Amoxicillin was effective as an initial treatment.
Keywords: Community Pneumonia; Pediatric Patients; Risk Factors; Symptoms; Treatment.
RESUMEN
La neumonía adquirida en la comunidad (NAC) es una causa relevante de morbilidad en niños menores de 10 años. Este estudio en el Centro de Salud Provincial N°48 de Rosario, Argentina, analizó la frecuencia de NAC en niños de 5 a 12 años durante 2023, empleando historias clínicas de 30 pacientes. El 53 % eran niñas y el 47 % niños, con edad promedio de 8,37 años. Los principales factores de riesgo fueron asma, hiperreactividad bronquial e infecciones respiratorias recurrentes (40 %), desnutrición (33 %) y nacimiento prematuro (20 %). Los síntomas comunes incluyeron fiebre, tos productiva y escalofríos. El 90 % de los casos recibió tratamiento con Amoxicilina oral. Se concluye que la frecuencia de NAC fue baja (4 %) y que la Amoxicilina fue efectiva como tratamiento inicial.
Palabras clave: Neumonía de la Comunidad; Pacientes Pediátricos; Factores de Riesgo; Síntomas; Tratamiento.
INTRODUCTION
Community-acquired pneumonia (CAP) is a significant cause of morbidity and mortality in children under 10 years of age.(1) In recent years, an increase in the incidence of complicated pneumonia in children has been observed.(2) In Latin America, CAP represents a significant burden on child health. The incidence of CAP in the region varies between 0,21 and 3600 cases per 100 000 children under 5 years of age, highlighting the importance of this disease in the pediatric population.(3,4)
CAP is a significant health problem in Argentina, especially in the infant population. According to a study, respiratory diseases, mainly pneumonia, are the third leading cause of mortality in children under one year of age and children under 5 years of age. Childhood pneumonia can be fatal if not properly treated, and it has been observed that the economic crisis that affected the country in 2001 increased the risk of mortality. Providing free medication at the first level of public health care for childhood pneumonia effectively reduces mortality and associated costs.(5)
Diagnosis in children under 10 years of age with CAP is based on clinical evaluation, physical findings, and, in some cases, complementary tests. Children with CAP may present with fever, tachypnea, dyspnea, cough, wheezing, chest pain, abdominal pain, and/or vomiting.(6,7) Careful clinical evaluation is essential for diagnosis, and in some cases, additional tests such as chest radiographs, blood tests, and laboratory tests may be performed to identify the causative agent. In resource-limited areas, diagnosing CAP solely by the presence of physical findings, such as fever, cough, refusal of food, and/or respiratory distress, is acceptable.(8)
It has been observed that factors such as malnutrition, prematurity, and certain infections make children more vulnerable to pneumonia, with agents such as Streptococcus pneumoniae and Enterobacter cloacae common in the Latin American region. In addition, it has been established that about 81,6 % of pneumonias in children are viral in origin, and 32,14 % are nosocomial in origin.(9) Treatment varies according to severity and the causative agent, including antibiotics, antivirals, or antifungals. It is critical that at-risk children, such as those with compromised immune systems or heart or lung disease, receive recommended vaccines to prevent pneumonia. Most children get better in 7 to 10 days with treatment, but those with severe pneumonia may need treatment for 2 to 3 weeks.(10)
Pneumococcal and influenza vaccines are the main preventive tools available against CAP, establishing themselves as a crucial measure to improve immunization and reduce mortality in the pediatric population in Argentina and throughout Latin America.(11) It is important to note that childhood pneumonia remains one of the leading causes of mortality in this population, which underlines the importance of prevention, early diagnosis and adequate treatment.(12)
Currently, there are few studies describing the frequency of CAP in Argentina. Bernstein and Drake 2009 evaluated the health impact and costs of the free provision of drugs at the first level of public health care for childhood pneumonia. In this study, 15 001 041 prescriptions of pediatric patients with respiratory system diseases were analyzed; 1 % (47 480 prescriptions) of children under 15 years of age were diagnosed with CAP. In children under 5 years of age, the diagnosis of CAP was 1,1 % and 0,8 % in children under 1 year of age.(5) While the study by Ensinck et al. shows that out of 54 pneumonias due to Staphylococcus aureus, 85 % were CAP. Likewise, an increase in the rate of CAP pneumonias from 4,9 cases per 10 000 patients in 2008 to 10 cases per 10,00 discharges in 2017 is observed. Positing that the prevalence of CAP pneumonias doubled during the last decade.(13)
Because of this, the present study asks the question: What is the frequency of community-acquired pneumonia in children aged 5 to 12 years in the Provincial Health Center No. 48 of the city of Rosario, Argentina, in 2023?
METHOD
The study was quantitative, descriptive, cross-sectional and retrospective. The study lasted six months from September 2023 to March 2024.
The research was carried out at the Provincial Health Center N°48, located at Nochetto 693, Antártida, in the city of Rosario, province of Santa Fe, Argentina. It is a first level health center, of public character and municipal administration. It offers daily medical attention in the following specialties: general surgery, medical clinic, nursing, gynecology, immunizations, general and/or family medicine, obstetrics and pediatrics.
The population consisted of all pediatric patients who attended the Provincial Health Center N°48 for medical care during the year 2023. The following selection criteria were applied to them:
Inclusion criteria
· Patients of both sexes; aged between 5 and 12 years; with a diagnosis of CAP recorded in the clinical history, and who had a chest X-ray.
Exclusion criteria
· Pediatric patients with respiratory conditions and symptoms associated with CAP without diagnostic confirmation (absence of diagnostic studies).
· Diagnosis of other lower respiratory tract infections other than CAP.
The sampling was non-probabilistic and was conducted by convenience sampling, with the consecutive incorporation of all cases.
A review of the patients' clinical histories was carried out as a data collection instrument to collect data on age, sex, risk factors present, diagnostic studies, and treatment used for CAP.
The statistical analysis consisted of a descriptive analysis of the quantitative variables through absolute and relative percentage frequencies. It was summarized through central position measures: mean, median, and mode, non-central position measures: quartiles 1 and 3, and dispersion measures: range and standard deviation. In comparison, qualitative variables were analyzed through absolute and relative percentage frequencies. From these summaries, graphs were constructed with the Excel program and tables for easy visualization.
The principles established in the Declaration of Helsinki and the Personal Data Protection Law (Law 25,326), applicable throughout the national territory, were respected, reserving the identity and the data obtained, ensuring the anonymity and confidentiality of the patients. Authorization was obtained from the health center authorities to carry out the study.(14,15)
RESULTS
A total of 30 medical records of pediatric patients diagnosed with CAP were reviewed. Of these 53 % (n=14) were female and 47 % (n=16) male; with a mean age of 8,37 ± 2,51 years (min.3; max. 12) (figure 1).
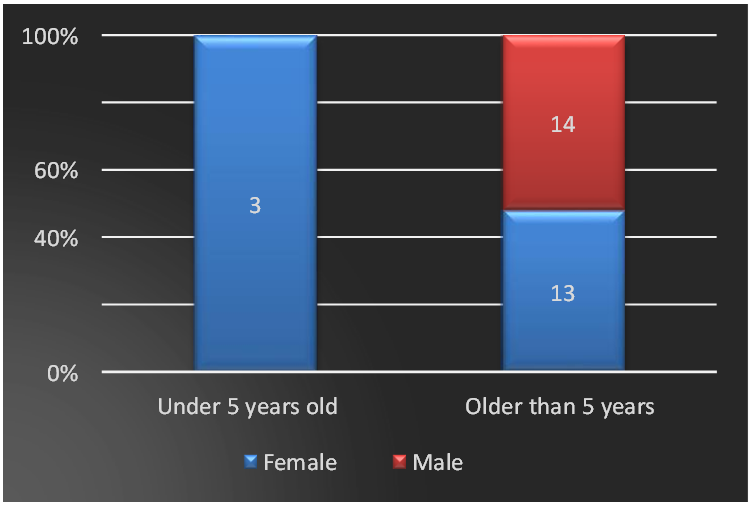
Figure 1. Frequency of patients according to sex and age range
When identifying the risk factors associated with the frequency of CAP, it was found that 40 % of the cases presented asthma, bronchial hyperreactivity and recurrent respiratory infections, 33 % malnutrition, 20 % premature birth, 10 % chronic diseases, 7 % attended day care centers and 3 % lived in overcrowded conditions (figure 2).
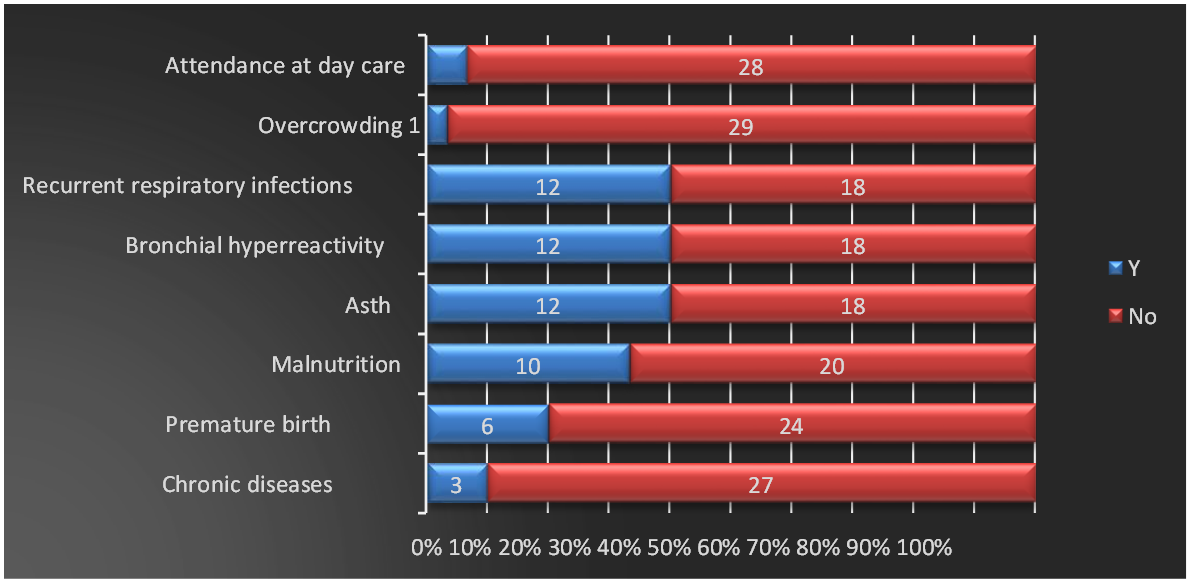
Figure 2. Risk factors associated with the frequency of community-acquired pneumonia
Symptoms associated with the diagnosis of the disease included a gradual onset, fever greater than 38,5°, productive cough, chills, myalgias and arthralgias (figure 3).
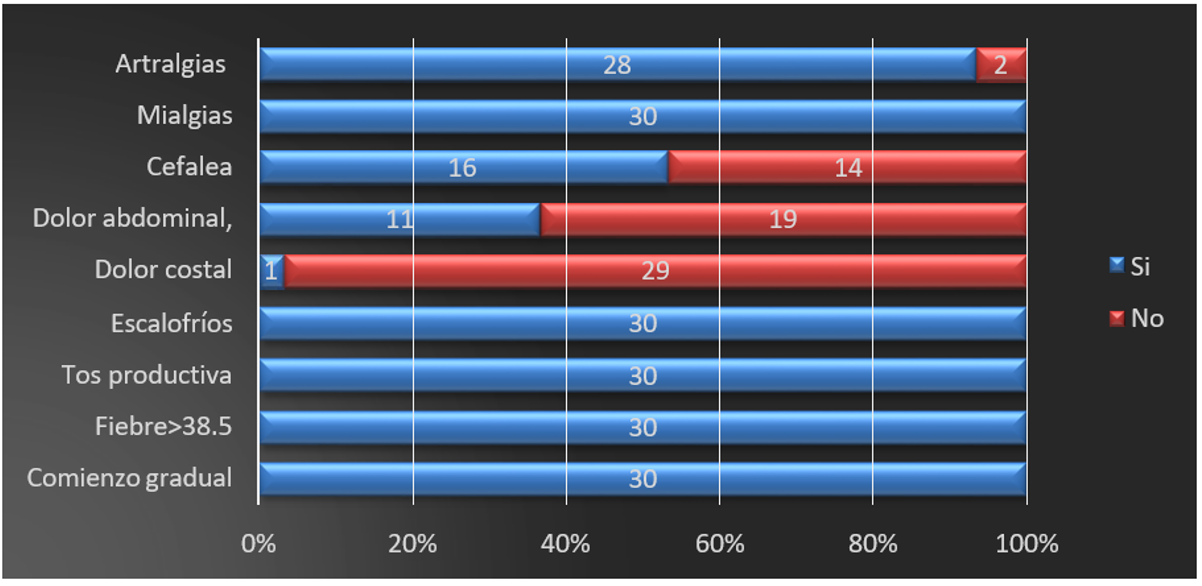
Figure 3. Symptoms associated with the diagnosis of community-acquired pneumonia
The following diagnostic methods were used to diagnose CAP:
· Chest X-ray accompanied by laboratory tests in 100 % of cases.
· Lobar condensation in 67 % of cases.
· Computed tomography, chest X-ray and lobar condensation in 3 % of cases, finding the presence of pleural effusion.
The treatment used in 90 % of the cases was Amoxicillin orally in doses of 80-100mg/kg every 8 hours for 7 days. One case required the use of Cefuroxin in combination with clarithromycin (figure 4).
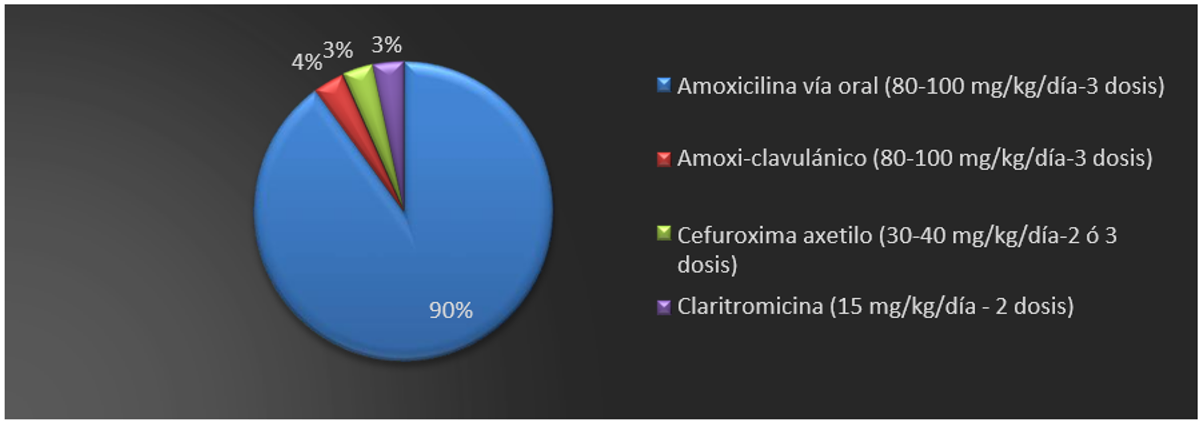
Figure 4. Treatment used
DISCUSSION
The frequency of CAP in the Provincial Health Center N°48 of the city of Rosario in the year 2023 was 4 %, showing similarity with the findings by Ensinck, who proposes an annual rate of pneumonia concerning hospital discharges of 4,9 cases per 10 000 children for 2008 and of 10,1 cases per 10 000 children for 2017.(13)
In Argentina, respiratory diseases, mainly pneumonia, are the third leading cause of mortality in children between 1 and 5 years of age. One study estimated that the free provision of drugs for CAP at the first level of public health care could have prevented deaths and years of life potentially lost in children under 5 years of age.(5) Therefore, it can be said that pediatric CAP represents an essential burden of disease in Argentina, with high incidence, hospitalization, and mortality rates, especially in children under 5 years of age. Improving etiological diagnosis and access to timely and quality antibiotic treatment are key to reducing its impact.
The results observed a higher frequency of females than males, a variable pattern indicated by the Peruvian Society of Infectious and Tropical Diseases.(16)
According to the studies reviewed, several risk factors are associated with a higher frequency of CAP. Among the host factors are chronic diseases, prematurity, social problems, malnutrition, asthma, bronchial hyperresponsiveness, recurrent respiratory infections, and a history of acute otitis media requiring tympanostomy tubes.(17,18) Coinciding with the risk factors identified in the study, the presence of asthma, bronchial hyperresponsiveness, and recurrent respiratory infections stands out.
Moreover, overcrowding, including daycare attendance, passive smoking, or exposure to environmental pollutants, has a recognized impact on respiratory infections in children. Several previously cited factors have also been significantly associated with increased morbidity or mortality in CAP.(19) Daycare attendance and overcrowding were also reported as risk factors in the population studied.
In addition, the pediatric patients evaluated presented symptoms associated with the diagnosis of CAP, such as fever greater than 38 degrees, productive cough, chills, myalgia, arthralgia, headache, and abdominal pain. This coincides with the available literature, which states that children with CAP may present fever, tachypnea, dyspnea or respiratory distress, cough, wheezing, and/or chest pain. Occasionally, they are accompanied by abdominal pain and/or vomiting and headache.(20)
Fever is considered an essential sign of CAP in infants. It has been described that high fever (38,4°C) in the first 72 h after admission is more frequently associated with a bacterial or mixed etiology and a higher level of severity of the disease. However, no clinical value has been found for the fever pattern before the child's initial assessment. On the other hand, the absence of fever has been attributed a negative predictive value of 97 %.(21)
Likewise, cough can be dry or productive, assuming it is productive on many occasions, especially in children, and it is the one that prompts us to mobilize secretions. Chest pain is a symptom generally referred to by the older child and is usually associated with pleuritis and/or pleural effusion. In younger children, general clinical signs of lower respiratory tract involvement on physical examination, such as nasal flaring, tachypnea, dyspnea, and retractions, are more specific for diagnosing lower respiratory tract infection than fever and cough.
Therefore, Madurga et al. (2011) explain that pneumonia's presentation varies according to age, causative agent, and immune status. It is characterized by general symptoms such as fever, chest pain, headache, malaise or vomiting, and respiratory symptoms such as rapid breathing, cough, shortness of breath, and lung auscultation abnormalities such as crackling sounds and a tubal murmur. Tachypnea, which is rapid breathing, is considered one of the most specific signs of lower respiratory tract infections, and its absence makes a diagnosis of pneumonia unlikely.(22,23)
For treatment, in this work, in 90 % of the cases, Amoxicillin was used orally in doses of 80-100mg/kg every 8 hours for 7 days of treatment, or Amoxicillin in combination with clavulanic acid with the same doses and duration. However, one of the cases required Cefuroxin combined with clarithromycin. These treatment regimens coincide with the literature, expressing that the recommended duration of antibiotic treatment in a patient with typical CAP without complications and not requiring admission is 7 days (Moreno-Pérez et al., 2015). Likewise, the first-line antibiotics for outpatient treatment are Amoxicillin or amoxicillin-clavulanic acid, 13, coinciding with the treatment provided to the patients in the present study.
According to Martín et al., it is important to differentiate between bacterial and viral causes of pneumonia to provide adequate treatment, avoid unnecessary antibiotic use, and prevent possible complications of bacterial pneumonias. For this reason, numerous studies are being conducted on nonspecific tests and acute-phase reactants to help determine the cause and/or severity of community-acquired pneumonias.
Similarly, Korppi et al. have indicated that Mycoplasma pneumoniae is a common cause of pediatric CAP in primary health care, and co-infections with Streptococcus pneumoniae are common.(24) Both S. pneumoniae and M. pneumoniae should be considered when initiating antibiotic treatment in children with this pathology. Therefore, treatment of pediatric CAP is based on oral or intravenous antibiotics according to severity, lasting 7 days in ambulatory cases. Pneumococcal vaccination and other preventive measures are key to reducing the disease burden.(25)
CONCLUSIONS
A low frequency of CAP (4 %) was found in pediatric patients under 12. Asthma, bronchial hyperresponsiveness, and recurrent respiratory infections were risk factors in the studied population. Clinical manifestations of CAP were fever higher than 38,5°, productive cough, chills, myalgias, and arthralgias. Amoxicillin was used orally at a dose of 80-100mg/kg every 8 hours for 7 days as the first treatment option.
Limitations
This was a retrospective study in which secondary sources were used for data collection, making underreporting possible. Likewise, being a unicentric study, the risk factors and clinical manifestations reported in the present study cannot be associated with the diagnosis of all cases of CAP reported in the various health centers of the city of Rosario.
BIBLIOGRAPHIC REFERENCES
1. de Benedictis FM, Kerem E, Chang AB, Colin AA, Zar HJ, Bush A. Complicated pneumonia in children. Lancet Lond Engl 2020;396:786-98. https://doi.org/10.1016/S0140-6736(20)31550-6.
2. Moreno-Pérez D, Andrés A, Tagarro A, Escribano A, Figuerola J, García JJ, et al. Neumonía adquirida en la comunidad: tratamiento ambulatorio y prevención. An Pediatr 2015;83:439 1-439 7. https://doi.org/10.1016/j.anpedi.2014.10.028.
3. Giménez Sánchez F, Sánchez Marenco A, Battles Garrido JMa, López Soler JA, Sánchez-Solís Querol M. Características clínico-epidemiológicas de la neumonía adquirida en la comunidad en niños menores de 6 años. An Pediatría 2007;66:578-84. https://doi.org/10.1157/13107392.
4. Visbal Spirko LP, Galindo López J, Orozco Cepeda K, Vargas Rumilla MI. Neumonía adquirida en la comunidad en pediatría. Rev Científica Salud Uninorte 2007;23.
5. Bernztein R, Drake I. Neumonía de la comunidad en niños: impacto sanitario y costos del tratamiento en el primer nivel de atención público de la Argentina. Arch Argent Pediatr 2009;107:101-10. https://doi.org/10.5546/aap.2012.101.
6. Ahn JG, Cho H-K, Li D, Choi M, Lee J, Eun B-W, et al. Efficacy of tetracyclines and fluoroquinolones for the treatment of macrolide-refractory Mycoplasma pneumoniae pneumonia in children: a systematic review and meta-analysis. BMC Infect Dis 2021;21:1003. https://doi.org/10.1186/s12879-021-06508-7.
7. Cui X, Zhao Z, Zhang T, Guo W, Guo W, Zheng J, et al. A systematic review and meta-analysis of children with coronavirus disease 2019 (COVID-19). J Med Virol 2021;93:1057-69. https://doi.org/10.1002/jmv.26398.
8. Martín A, Moreno-Pérez D, Alfayate S, Couceiro JA, García ML, Korta J, et al. Etiología y diagnóstico de la neumonía adquirida en la comunidad y sus formas complicadas. An Pediatr 2012;76:162 1-162 18. https://doi.org/10.1016/j.anpedi.2011.09.011.
9. Martínez Santander CJ, Flores Paredes SA, Pesantez Ferreira AD, Suquinagua Ortiz MD, Bravo Vázquez CA, Guevara Carvajal MC. Prevalencia de la neumonía en pacientes pediátricos en Latinoamérica durante el periodo 2017-2022. Mediciencias UTA 2022;6:108-22. https://doi.org/10.31243/mdc.uta.v6i4.1819.2022.
10. González J, Julián-Jiménez A, Candel FJ, Urgencias. IdISSC. Hospital Clínico San Carlos. Madrid S, Spain. Community-acquired pneumonia: selection of empirical treatment and sequential therapy. SARS-CoV-2 implications. Rev Espanola Quimioter Publicacion Of Soc Espanola Quimioter 2021;34:599-609. https://doi.org/10.37201/req/144.2021.
11. Torres A, Cilloniz C, Niederman MS, Menéndez R, Chalmers JD, Wunderink RG, et al. Pneumonia. Nat Rev Dis Primer 2021;7:25. https://doi.org/10.1038/s41572-021-00259-0.
12. Redondo E, Rivero I, Vargas DA, Mascarós E, Díaz-Maroto JL, Linares M, et al. Vacunación frente a la neumonía adquirida en la comunidad del adulto. Posicionamiento del Grupo de Neumoexpertos en Prevención. SEMERGEN - Med Fam 2016;42:464-75. https://doi.org/10.1016/j.semerg.2016.07.009.
13. Ensinck G, Lazarte G, Ernst A, Romagnoli A, López Papucci S, Aletti A, et al. Neumonía por Staphylococcus aureus resistente a meticilina adquirido de la comunidad en un hospital pediátrico. Nuestra experiencia de 10 años. Arch Argent Pediatr 2021;119:11-7.
14. World Medical Association. Declaración de Helsinki: Principios éticos para las investigaciones médicas en participantes humanos. World Med Assoc 2024. https://www.wma.net/es/policies-post/declaracion-de-helsinki-de-la-amm-principios-eticos-para-las-investigaciones-medicas-en-seres-humanos/ (accedido 31 de octubre de 2024).
15. Senado y Cámara de Diputados de la Nación Argentina. Ley de Protección de los Datos Personales. 2000.
16. Sociedad Peruana de Enfermedades Infecciosas y Tropicales. Guía de práctica clínica: neumonía adquirida en la comunidad en niños. 1ra ed. Lima, Perú: OPS; 2009.
17. Davis Rocha C, Padilla R. Factores de riesgo socioculturales asociado a Neumonía Adquirida en la Comunidad desde la cosmovisión indígena Miskitu en niños menores de 5 años. Tesis de grado. Universidad de las Regiones Autónomas de la Costa Caribe Nicaragüense, 2020.
18. Kasundriya SK, Dhaneria M, Mathur A, Pathak A. Incidence and Risk Factors for Severe Pneumonia in Children Hospitalized with Pneumonia in Ujjain, India. Int J Environ Res Public Health 2020;17:4637. https://doi.org/10.3390/ijerph17134637.
19. Alberto Magaña SP. Perfil clínico y epidemiológico de pacientes de 3 meses a 12 años con diagnóstico de neumonía adquirida en la comunidad refereridos por necesidad de soporte ventilatorio al Hospital Nacional de Niños Benjamín Bloom, entre 1 de Enero 2012 y 31 de Deciembre 2017. Tesis de postgrado. Universidad de El Salvador, 2020.
20. Jullien S, Pradhan D, Tshering T, Sharma R, Dema K, Garcia-Garcia S, et al. Pneumonia in children admitted to the national referral hospital in Bhutan: A prospective cohort study. Int J Infect Dis IJID Off Publ Int Soc Infect Dis 2020;95:74-83. https://doi.org/10.1016/j.ijid.2020.04.017.
21. Chang TH, Liu YC, Lin SR, Chiu PH, Chou CC, Chang LY, et al. Clinical characteristics of hospitalized children with community-acquired pneumonia and respiratory infections: Using machine learning approaches to support pathogen prediction at admission. J Microbiol Immunol Infect 2023;56:772-81. https://doi.org/10.1016/j.jmii.2023.04.011.
22. Tsai T-A, Tsai C-K, Kuo K-C, Yu H-R. Rational stepwise approach for Mycoplasma pneumoniae pneumonia in children. J Microbiol Immunol Infect Wei Mian Yu Gan Ran Za Zhi 2021;54:557-65. https://doi.org/10.1016/j.jmii.2020.10.002.
23. Chee E, Huang K, Haggie S, Britton PN. Systematic review of clinical practice guidelines on the management of community acquired pneumonia in children. Paediatr Respir Rev 2022;42:59-68. https://doi.org/10.1016/j.prrv.2022.01.006.
24. Korppi M, Heiskanen-Kosma T, Kleemola M. Incidence of community- acquired pneumonia in children caused by Mycoplasma pneumoniae: serological results of a prospective, population-based study in primary health care. Respirology 2004;9:109-14. https://doi.org/10.1111/j.1440-1843.2003.00522.x.
25. Chapman TJ, Olarte L, Dbaibo G, Houston AM, Tamms G, Lupinacci R, et al. PCV15, a pneumococcal conjugate vaccine, for the prevention of invasive pneumococcal disease in infants and children. Expert Rev Vaccines 2024;23:137-47. https://doi.org/10.1080/14760584.2023.2294153.
FINANCING
The authors did not receive funding for the development of this research.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Julieta Ivana Passas.
Data curation: Julieta Ivana Passas.
Formal analysis: Julieta Ivana Passas.
Research: Julieta Ivana Passas.
Methodology: Julieta Ivana Passas.
Project management: Julieta Ivana Passas.
Resources: Julieta Ivana Passas.
Software: Julieta Ivana Passas.
Supervision: Julieta Ivana Passas.
Validation: Julieta Ivana Passas.
Visualization: Julieta Ivana Passas.
Editor - original draft: Julieta Ivana Passas.
Writing - proofreading and editing: Julieta Ivana Passas.