Management
of preeclampsia.
The
management of preeclampsia begins with the evaluation of the health status of
the pregnant woman and the fetus, performing a clinical evaluation of the
neurological, respiratory, cardiovascular, hematological, biochemical and renal
functions, as well as an evaluation of fetal well-being with electronic fetal
monitoring, biophysical profile and Doppler study of theand uterine arteries.
Pregnant women with preeclampsia in most cases require hospitalization for
adequate treatment of hypertension, prevention of seizures, optimization of
intravascular volume, maintenance of adequate arterial oxygenation, early
detection and/or treatment of complications (Department of ObstetricsUC of
Chile, 2020).
Management of preeclampsia without severity criteria.
Relative
rest, normocaloric, normoproteic and normosodic diet are recommended.
Do
not use antihypertensive drugs. The definitive treatment for preeclampsia is
termination of pregnancy. If the pregnant woman is 37 weeks or more, the
pregnancy should be terminated by vaginal delivery or cesarean section. If the
woman is less than 37 weeks old and there is no maternal or fetal compromise,
management over time is possible. Continue with general measures and closely
monitor the mother and fetus. If, despite treatment, arterial hypertension is
not controlled or if the disease progresses to severe preeclampsia, or if there
is preeclampsia or signs of fetal, hematologic, or renal distress, hepatic,
pulmonary, or neurologic dysfunction, the pregnancy will be terminated
immediately, regardless of gestational age (Guzman et al., 2018).
Management of preeclampsia with severity criteria
Preeclampsia
with severe criteria will progress to severe complications such as acute
pulmonary edema, renal failure, hypertensive encephalopathy with cerebral
hemorrhage, retinal detachment, placental abruption, subcapsular hematoma, or rupture
of the liver, HELLP syndrome, which can lead to death of the pregnant woman,
fetus or baby.
Therefore,
management should be timely, multidisciplinary, and effective. A pregnant woman
who presents vaginal bleeding and signs of placental abruption always suspects
preeclampsia as a background condition (Velumani et at., 2022).
In
preeclampsia there is a contraction of intravascular contents, unlike the usual
hypervolemia of the pregnant woman; there is a tendency to oliguria due to lack
of fluids, despite edema (Tacuri et al., 2022).
Adequate
intravascular expansion with 0,9 % saline should be ensured, in case oliguria
persists, initiate, followed by a diuretic such as furosemide in order to
achieve blood pressure normalization more rapidly and reduce the need for
antihypertensive therapy (Rojas et al., 2019).
Strict
water balance and monitoring of vital functions should be performed every 15
minutes. Initiate a venous infusion of magnesium sulfate for the prevention of
convulsions; this solution should be given with an initial attack dose, and it
is suggested to maintain the infusion for 24 hours after delivery. The
administration of magnesium sulfate should be suspended if tendon areflexia or
depression of consciousness is detected, and calcium gluconate should be
administered in this case. ́Antihypertensive treatment should only be used if
the systolic blood pressure is≥ 160 mmHg or if the diastolic blood pressure is≥
110 mmHg, in which case the following drugs are recommended: Labetalol,
Hydralazine, Methyldopa, Nifedipine (Calderon et al., 2023).
Nursing
role
Primary
nursing care includes continuous assessment and early identification of signs
of worsening disease. Adhering to the medical guideline: adequate expansion of
the endovascular line with 0,9 % saline, 50-60 drops/min for the first liter
should be ensured; and, if oliguria persists, the attending physician will
prescribe 500 ml of colloid solution on a rapid drip, followed by 10 mg of
furosemide intravenously. The diuresis should be monitored with a bladder
catheter connected to a Blood pressure, heart rate, respiratory rate, and
oxygen saturation should be monitored every 15 minutes (Gaona, 2021).
Start
an intravenous infusion of magnesium sulfate. The infusion solution is prepared
by combining five ampoules of 20 % magnesium sulfate (10 ml ampoules) with 50
ml 0,9 % saline. This solution provides 1 g of magnesium sulfate per 10 ml, and
it is recommended to administer 4 grams (40 ml) for 15-20 days as an initial
loading dose; continuous infusion of 1 g every hour (10 ml per hour) and
maintenance infusion for 24 hours after delivery. When using magnesium sulfate,
the knee reflex, respiratory rate, which should be at least 14 breaths per
minute, and urine output, no less than 25-30 ml/hour, should be monitored
(Gaona, 2021).
It
is also recommended that O2 saturation be monitored with pulse oximetry. The
administration of magnesium sulfate should be suspended if tendon hyporeflexia
is detected, if there is an alteration of consciousness, or if there is a
tendency for superficial or slow ventilation. In this case, the treating
physician will prescribe calcium gluconate, 1 to 2 grams intravenously.
Antihypertensive treatment should only be used if the systolic blood pressure
is≥ 160 mmHg or if the diastolic blood pressure is≥ 110 mmHg (Gaona, 2021).
Risk of alteration of the maternal-fetal dyad
Vulnerable
to disruption of the symbiotic relationship between mother and fetus due to
pregnancy-related comorbidities or conditions that may affect health (Heather
Herdman et al., 2021).
Risk factors for the risk of maternal-fetal dyad disruption
Some
of the risk factors are pregnancy complications such as multiple pregnancy,
threatened miscarriage, oligohydramnios, hemorrhage in the second and third
half of pregnancy. Other risk factors that can be mentioned are the drug
dependence, non-compliance with medical indications, inadequate prenatal care,
physical abuse, diabetes, among others (Chesya et al,. 2019).
Another
source mentions fetal oxygen transport compromise (oligohydramnios,
preeclampsia/eclampsia) as another important risk factor (Sacks et al., 2020).
Gestational
hypertension
Gestational
hypertension is high blood pressure during pregnancy. It occurs in
approximately 3 out of every 50 pregnancies. This condition is different from
chronic hypertension, preeclampsia and eclampsia. It is a blood pressure
problem during pregnancy that begins in the second half of pregnancy and
usually disappears after birth (Perez et al., 2019).
Pathophysiology of gestational hypertension
It
is caused by the rapid and severe elevation of blood pressure that produces two
Events: systemic endothelial dysfunction that causes decreased synthesis of vasodilator
agents (nitric oxide and prostacyclins) and increased synthesis of cytokines
and cell adhesion molecules. Microcirculation further increases blood pressure
and damages the vascular endothelium, causing fibrinoid necrosis and
endothelial proliferation. It also causes peripheral tissue ischemia in target
organs. The second affects the renin-angiotensin-aldosterone system by salt
concentration and plasma osmolarity, which increases sodium excretion by the
kidney, causing intravascular volume deficit (hypovolemia) that affects blood
flow and originating terminal organ dysfunction (Perez et al., 2019).
Risk of gestational hypertension
Risks
for gestational hypertension include: high blood pressure before or during a
previous pregnancy, kidney disease, diabetes, younger than 20 or older than 40,
multiple pregnancy (Mayo Clinic, 2022).
Symptoms of gestational hypertension.
The
most frequently reported symptoms are: High blood pressure during the second
half of pregnancy, headache, edema, weight gain, blurred or double vision,
nausea or vomiting, abdominal pain, pollakiurea, as also symptoms with less
prevalence are dizziness, conjunctival hemorrhage, tinnitus and epistaxis
(Stanford medicine children's health, 2022).
Complications gestational hypertension
The
constant assessment of the pregnant patient with hypertensive disorders should
be taken into account in order to avoid complications such as: Compromised
blood vessels, liver failure, renal failure, seizures, placental abruption,
insufficient fetal growth, stillbirth, maternal death (Velumani Et. at., 2022).
Treatment of gestational hypertension
́The objective is to lower blood pressure
without compromising perfusion of target organs, hemodynamic monitoring of the
pregnant woman and rapid venous access for the administration of antihypertensive
drugs (alfamethyldopa, hydralazine and labetalol); considering a systolic blood
pressure of 160 and a diastolic blood pressure of≥ 110 mm Hg with the
aim of stabilizing maternal-fetal health (Stanford medicine children's health,
2022).
Prevention of gestational hypertension
Early
diagnosis and treatment, periodic prenatal checkups.
Nursing care for pregnant women with hypertension
Nursing
care are the processes that are applied to reduce the complications of maternal
and fetal gestational hypertension, in order to preserve gestation. Among the
care for gestational hypertension, we can mention: Relative rest, periodic
monitoring of BP and fetal well-being, normocaloric, normoproteic and
normosodic diet, pharmacological treatment with labetalol, hydralazine and
alpha-methyldopa, termination of gestation, in cases more 37 weeks. If the
gestational age is less 34 weeks the lungs will be matured with
corticosteroids, do not stop the treatment just after delivery but reduce it
gradually (Garcia Lopez, 2020).
Theoretical basis of nursing care patients with preeclampsia
It
is believed that Hildegard E. Peplau's theoretical proposal aims to highlight
the psychological tasks that are developed in the nurse-patient relationship,
which depends on the nurse's ability to perceive and identify the difficulties
in her relationship with the patient and her ability to help them to solve
problems. Peplau analyzes the four stages of the nurse-patient relationship,
and these have been applied to the care of our patients with preeclampsia:
Orientation, identification, exploitation, and resolution (Machado et al.,
2021).
On
the other hand, Jean Watson argues that it is necessary to rescue the human,
spiritual, and transpersonal aspects of clinical nursing practice, elaborating
her theory "Of human care" based on seven basic assumptions. First,
care must be effective and interpersonal. Second, caring involves factors that
result from meeting human needs. Third, effective care promotes health and
personal growth. Fourth, the responses derived from caregiving accept the
person not only as he or she is but as the person can become. Fifth, a caring
environment offers the development of potential and allows the person to choose
the best action at any given time. Sixth, caring is more "health-gené
tic" than healing, and seventh, the practice of caring is fundamental for
nursing (Gaona Castillo, 2021).
METHOD
Study design
The
methodological approach of this study is a qualitative analysis, the type of
study is a single clinical case, applying the nursing care process (PAE) to
respond to objectives set out in the research on the risk factors of the
patient with twin gestation, preeclampsia and collaborative problem Gestational
hypertension.
Subject
of study
A
33-year-old female patient, with twin gestation of 30 weeks at her last
menstrual period, with a medical diagnosis of preeclampsia, presenting fever,
headache, pelvic pain, swollen legs, foul-smelling vaginal discharge and
presence of blood without clots, vulnerable to present maternal-fetal
complications.
Scope
and period of the study
The
study period was performed in the gynecology service, attended from September 9
to 16, 2022.
Data
collection procedure
Source of information
The
following was used as a data collection instrument:
Reception
of verbal information from the patient with initials F.E.H.M., 33 years old.
Direct observation of the patient.
Personal
interview with the immediate family member (spouse).
Relevant
data from the patient's medical history: Medical progress record data, nursing
notes record data, diagnostic media results.
Performance
of the physical examination and comparison of data with the assessment tables.
Nursing assessment according to Marjory Gordon's 11 functional patterns.
Bibliographic
review of scientific evidence by other authors from the following sources:
Science, Direct, Scielo, Scielo, Elsevier, Google academic, NANDA International
2021-2023, videos through the keywords such as: nursing care, twin gestation,
preeclampsia.
Information procedure
In
order to proceed with the data collection, prior authorization was required
from the patient and the personnel responsible for the gynecology service of
the clinic, guaranteeing the process of protection and confidentiality of the
data provided for study.
Collection of information
It
was carried out in 4 phases:
·
First
phase: reviewing the patient's clinical history to extract clinical data such
as: personal history, family history, reason for consultation, results of
auxiliary examinations, main medical diagnosis, medical evolution, nursing
diagnoses and the evolution nursing care.
·
Second
phase: The nursing assessment is carried out through a personal interview,
following Marjory Gordon's 11 functional patterns assessment guide, using the
identification and recognition of the main nursing diagnosis for the
development of an individualized nursing care plan for the case under study.
·
Third
phase: The patient was followed up twice on her first day of hospitalization in
the gynecology department to assess the evolution of the pregnant woman.
·
Fourth
and last phase: an exhaustive review of the scientific evidence was carried
out, setting limits according to date criteria and limiting the search for
information from 2019 to the present. Databases were used: Science, Direct,
Scielo, Elsevier, Google Scholar, NANDA International 2021-2023, and videos
through keywords such as Nursing, twin gestation, and preeclampsia.
Data
processing
Data
processing and analysis was carried out in three stages: First moment: based on
the assessment guide of the 11 functional patterns of Marjory Gordon, we
proceeded to the realization of a reasoning network based on the "AREA
Model". Developed by Pesut and Herdman, for the selection of the main nursing
diagnosis according to the NANDA-I taxonomy 2021-2023.
Second
moment: after the choice of the DxEP, we proceeded to the establishment of the
outcome criteria (NOC) and interventions (NIC) and the selection and
prioritization of the nursing activities.
Third
moment: after the execution of the programmed nursing activities, we proceeded
to the evaluation of the PAE, with the objective of verifying the effectiveness
of the interventions carried out in the nursing care plan for a patient with
twin gestation, preeclampsia and a collaborative problem of gestational
hypertension.
RESULTS
Case description
A
young adult patient with the initials HMFE, female, 33 years old, from the
district of Miraflores, with higher university education, business administrator
occupation, was admitted to the emergency area, accompanied by her husband for
presenting a temperature of 38,7 °C, headache, tinnitus, abdominal pelvic pain,
edema of the lower limbs, vaginal discharge without clots with bad odor and
blood. On medical evaluation, she was diagnosed with a twin pregnancy of 30
weeks by the date of her last menstrual period and probable preeclampsia.
Hospitalized in the gynecology department, she is in absolute rest, in an
antalgic position, with permanent monitoring of vital functions and initiation
of medical therapy.
Family history
Mother: Cervical cancer and hypertensive. Father:
Diabetic and hypertensive.
Personal background
Drug allergies: NSAIDS
Food allergy: Lactose intolerant, shellfish allergy.
Metals: Denies
Allergic rhinitis: Denies Bronchial asthma: Denies
Toxic habits
Tobacco:
Denies Alcohol: Denies Coffee: Denies
Other
toxics: Denies
Pathological
history
Arterial
hypertension, diagnosed in her first pregnancy, with regular treatment of methyldopa
250 mg every 8 hours.
Hypothyroidism
diagnosed 3 years ago, with usual treatment levothyroxine 75 mcg every 24
hours.
Gynecological history
Menarche at 12 years of
age. FUR: 22.03.22
Gestations:
2
Use
of contraceptive methods: Denies History of PCOS/EPI: Yes
Usual
medication for her current pregnancy: Gestavit DHA, folic acid.
Epidemiological history of STD
Denied Contact TB:
Denied
Vaccinations
in the last year: Covid 19 Occupation: Administrator Physical activity: Denied
Surgical
history
Uterine
curettage (2020)
Colelap
Surgery (2018)
Breast
Augmentation Surgery (2012) PO Liposuction (2012)
Current
situation: on evaluation, patient lucid, oriented
in time, space and person, Glasgow 15 points, responds to all stimuli, is alert
and vigilant, refers intense headache on a scale of EVA 10/8, ventilating
spontaneously at a FIO2: 0. 21 %, with pale skin, hydrated skin and mucous
membranes, normal sweating. 21 %, with pale skin, hydrated skin and mucous
membranes, normal sweating, distended soft abdomen, pregnant uterus, refers
pain in the abdominal-pelvic region in VAS 10/8 points, wanders with limitation
due to some weakness in lower limbs, edema in lower limbs +++, spontaneous
bladder and bowel elimination, vaginal discharge with bad odor and evidence of
slight bleeding.
Medical
diagnosis: nulliparous second gestation of 30s x
LMP, twin pregnancy, biamniotic, high risk of preterm delivery, risk of chorioamnionitis, preeclampsia.
Medical
therapeutics
Soft,
low sodium diet Absolute rest Strict water balance Bleeding control
Monitoring
of vital signs every 2 hours Fetal monitoring every 4 hours
Parenteral
hydration of sodium chloride 0,9 % Methyldopa 250 mg orally every 8 hours.
Nifedipine
30 mg/day orally PRN a Blood pressure greater than 160/100 mmHg,
Gentamicin
320 mg intravenous every 24 hours. Clindamycin 600 mg intravenous every 8
hours. Ceftriaxone 2 grams intravenous every 24 hours. Simeticone 180 mg orally
after meals. Omeprazole 40 mg intravenous every 24 hours.
Paracetamol
1 gram intravenous PRN at temperature greater than or equal to 38 °C.
Laboratory
tests
Leukocytes:
12,440 Cells/uL (Normal values: 4,500 - 11,000 Cells/uL)
Hematocrit:
33,2 % (Normal values: 36 - 43 %)
Platelets:
160,000,0 Cells/uL (Normal values: 150,000 - 475,000 Cells/uL)
Hemoglobin:
9,8 g/dl (Normal values: 12 -16 g/dl)
Creatinine:
1,5 mg/dl (Normal values: 0,5 - 0,9 mg/dl)
Urea:
52 mg/dl (Normal values: 17 - 49 mg/dl)
Protein:
8,3 g/dl (Normal values: 6,0 - 8,3 g/dl)
Glycemia:
85 mg/dl (Normal values: 70 - 100 mg/dl) SARS-CoV-2 ANTIGEN: Negative.
Hepatitis
B Australian Antigen (HBsAg): Non reactive, HIV Ac (HIV 1-2 Antibodies): Non
reactive.
Group
and Factor: A negative
Case
evaluation
After
introducing my patient according to her clinical report I proceed to assess her
according to Marjory Gordon's Eleven Functional Patterns of Health (PFS)
(Gordon, 1999):
Perception pattern - Health management
Nulliparous
second gestation patient with current twin gestation of 30 weeks, with a
history of an abortion in 2020, with obstetric ultrasound result of placental
accretism, altered laboratory results:
Leukocytes:
12,440 cells/uL
Hematocrit:
33,2 %.
Platelets:
160,000,0 Cells/Ul.
Hemoglobin:
11,8 g/dl.
Creatinine:
1,3 mg/dl.
Urea:
52 mg/dl.
Blood
glucose: 83 mg/dl.
SARS-CoV-2
ANTIGEN: Negative.
Hepatitis
B Australian Antigen (HBsAg): Non reactive.
HIV
Ac (HIV 1-2 Antibodies): Non reactive.
Group
and Factor: A negative.
Nutritional - metabolic pattern
Feverish
patient (temperature 38,7), with warm skin, pain in the abdomen, weight: 75 kg,
height: 168 cm, BMI: 26,6 (overweight), independent in her diet, eats 5 meals a
day, has been gaining weight in the last two months in the last two months. He
consumes liquids frequently, 2 ½ liters per day.
Additional
supplements consumed during pregnancy: Gestavid DHA 1 tablet orally every 24
hours and folic acid 10 mg orally every 24 hours.
Allergies
to shellfish, Lactose intolerant.
Good
swallowing of food. No nausea or vomiting, nor has he presented them in the
last few days.
Pale
skin, mucous membranes hydrated.
Pattern elimination
No
data is evident.
Activity - exercise pattern
Blood
Pressure: 190/110 mmHg, Heart Rate: 105 beats per minute.
Respiratory
rate: 22 breaths per minute, SpO2: 99 %. Rhythmic pulse, no heart murmur.
Eupneic
at rest. Intolerant to physical activity due to his condition.
Remains
in bed in an antalgic position, mobilized only for physiological elimination.
Patient
with limited gestational ambulation and weakness in lower limbs due to edema
and pain.
Edema
in both lower limbs++ ranging from thighs to feet. Carrier of peripheral line
N° 20 in dorsum of hand of left upper limb.
Rest - sleep pattern
No
data is evident.
Cognitive-perceptual pattern
Lucid
patient, oriented in time, space and person.
At
the GLASGOW 15-point scale assessment, patient responds to all stimuli, is
vigilant and alert.
No
language, memory or hearing problems. cognitive impairment.
She
refers headache and pelvic pain, to the assessment of VAS scale 10/8.
Self-perception - self-concept pattern
Patient
presents signs of anxiety, anguish, fear, nervousness, headache.
She
is aware of her current disease: hypertension, she is aware of the health risk
she presents, so she frequently requests information about her health status
and that of her babies.
She
feels loved and supported by her husband.
Role pattern - relationships
Married,
currently living with her husband. She receives support from both families.
Sexuality - reproduction pattern
Pregnant
with twins at 30 weeks. She had a previous pregnancy 2 years ago, which
culminated in a uterine curettage. Planned pregnancy with medical follow-up.
Congestive
breasts. Genitalia with vulvar edema, vaginal bleeding without clots 8 hours
ago without bad odor, no loss of amniotic fluid. Blood group and blood factor:
A positive.
Adaptation pattern - stress
The
patient and her husband, very distressed, report being very afraid of losing
their babies. They are very cooperative with the treatment indicated by the
gynecologist and the care plan required.
Values-beliefs pattern
Practicing
Catholic.
Care
plan
Diagnosis
Identification
of nursing diagnoses
Nursing
diagnoses were formulated using the NANDA taxonomy (Heather Herdman et
al.,2021).
Pattern
Perception - Health Management
(00126).
Poor knowledge r/c anxiety m/p request for information on health.
Definition:
Absence of cognitive information related to a specific subject, or its
acquisition.
Domain
5: Perception/cognition
Class
4: Cognition.
Nutritional
- Metabolic Pattern
(00007).
Hyperthermia r/impaired health status m/p temperature 38. 7°C.
Definition:
Core body temperature above the normal diurnal range due to failure of
thermoregulation.
Domain
11: Safety/protection Class 6: Thermoregulation Activity-Exercise pattern.
(00204)
Ineffective peripheral tissue perfusion r/c hypertension m/p elevated blood
pressures (BP: 160/98 mmHg)
Definition:
Decreased blood flow to the periphery, which may compromise health.
Domain
4: Activity/rest
Class
4: Cardiovascular/pulmonary responses.
(00303).
Risk of falls e/p decreased lower extremity strength due to edema and pain.
Definition:
Adult susceptible to experiencing an event that results in inadvertently
resting on the floor, ground or other lower level, which may compromise health.
Domain
11: Safety/protection. Class 2: Physical injury.
Cognitive
- Perceptual Pattern
(00132).
Acute pain r/c agents of biological damage m/p headache and abdominal pain. pelvic.
Definition:
Unpleasant sensory and emotional experience associated with actual or potential
tissue damage, or described in terms of such damage (International Association
for the Study of Pain); sudden or slow onset of any intensity from mild to
severe with an anticipated or predictable end, and lasting less than 3 months.
Domain
12: Physical comfort Class 1: Comfort
Pattern
Self-perception - Self-concept
(00148).
Fear r/unfamiliar situation m/p nervousness and fear
Definition:
Basic and intense emotional response to the detection of an imminent threat,
which implies an immediate alarm reaction.
Domain
9: Stress coping/tolerance.
Class
2: Coping response.
Sexuality
- Reproduction Pattern
(00209).
Risk of alteration of the maternal-fetal dyad and / or complications in
pregnancy.
Definition:
Vulnerable to disruption of the symbiotic relationship between mother and fetus
due to comorbidities or pregnancy-related conditions that may affect health.
NANDA-I Taxonomy, (Heather Herdman et al.,2021)
Domain
8: Sexuality
Class
3: Reproduction
(00206).
Risk of bleeding and / or pregnancy complications (Vaginal bleeding)
Definition:
Susceptible to a decrease in blood volume, which may compromise health.
Domain
11: Safety/Protection Class 2: Physical Injury
Adaptation
Pattern - Stress Tolerance
(00146).
Anxiety r/ stressors m/p changes in health status.
Definition:
An emotional response to a diffuse threat in which the individual anticipates
an unspecified imminent danger, catastrophe or misfortune.
Domain
9: Coping/stress tolerance. Class 2: Coping response.
Prioritized
nursing diagnoses
After
exposing the different nursing diagnoses that my patient has, I am going to
prioritize the main Nursing Diagnosis (DxEp) by means of a clinical reasoning
network based on the AREA Model (Pesut & Herman, 1999). The model
establishes clinical reasoning networks, based on the relationships that are
established between a number of the high number of diagnoses resulting in the
most accurate and appropriate diagnosis for each clinical case.
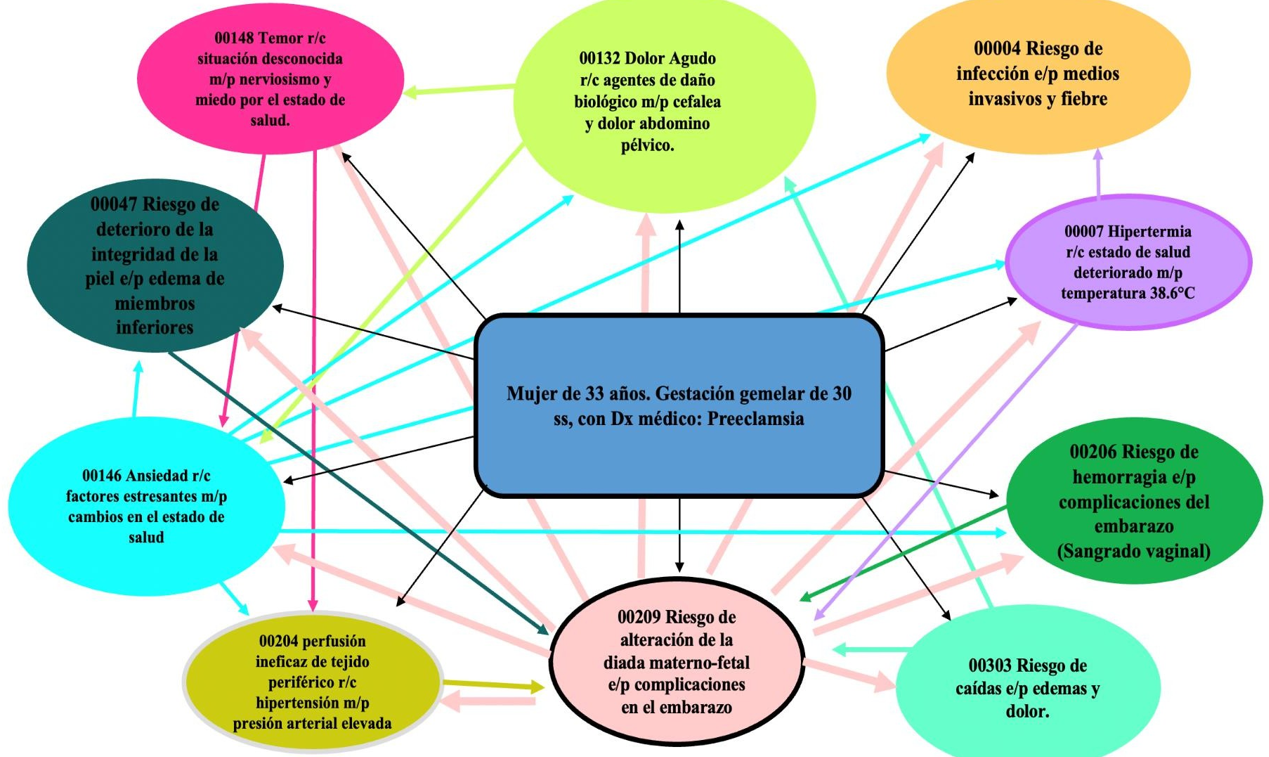
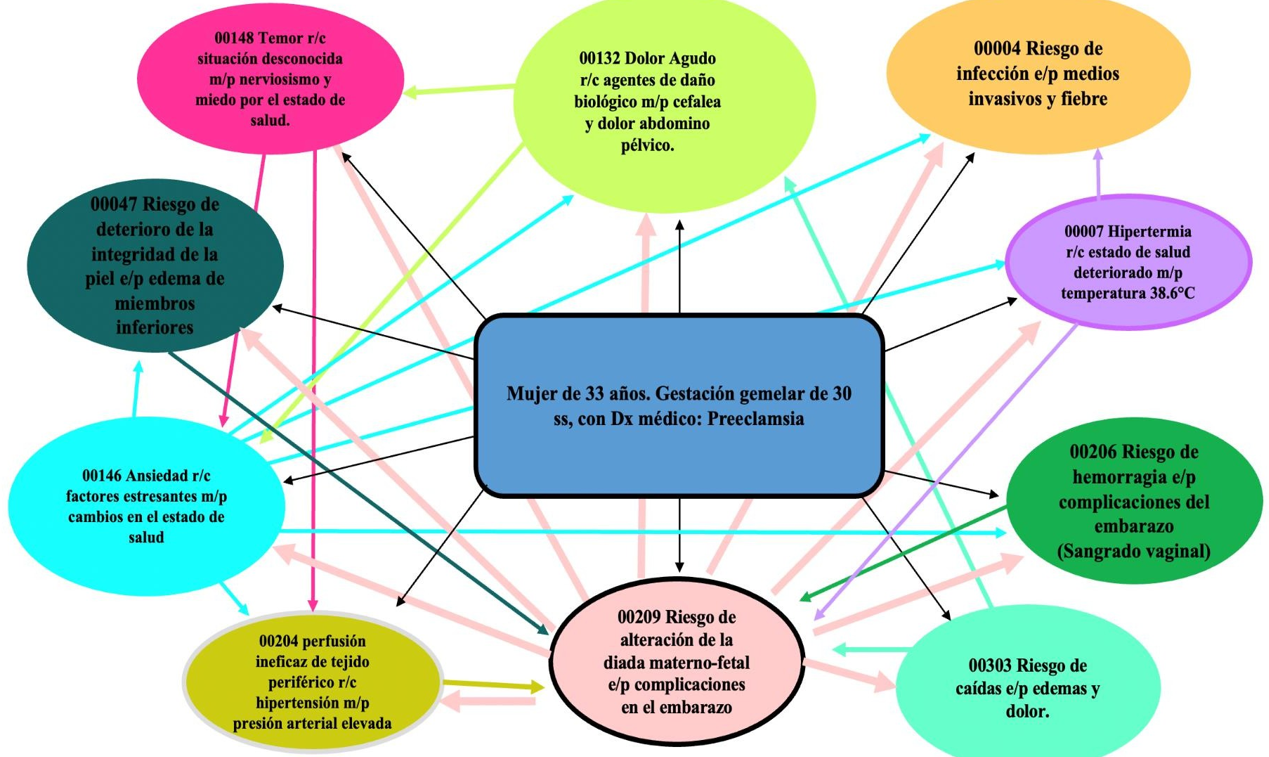
Figure 1.
DxE network
Primary Nursing Diagnosis (DxEp)
After
making the interrelation of the diagnoses proposed for the case, we can see in
Figure N°1 the choice of the main nursing diagnosis:
(00209).
Risk of alteration of the maternal-fetal dyad evidenced by complications in
pregnancy due to multiple gestation.
Definition:
Vulnerable to disruption of the symbiotic relationship between mother and fetus
due to comorbidities or pregnancy-related conditions that may affect health.
NANDA-I Taxonomy, (Heather Herdman et al.,2021).
Domain
8: Sexuality.
Class
3: Reproduction.
Justification
of the Main DxE
Currently,
the probability of multiple pregnancies has increased considerably due to the
delay in childbearing and the use of assisted reproductive techniques (Rodrigo,
Aparicio Caballero, & Salvador, 2022).
A
multiple pregnancy is considered a risky pregnancy, both for the mother and
fetus, due to the various anatomical and physiological changes that the body
undergoes throughout gestation (Stanford Medicine, 2022).
Multiple
pregnancies are complicated due to the large volume occupied by the gestation
of more than one baby. The uterus supports an excess of weight and can distend
exerting more pressure on the rest of the organs, the placenta grows more than
expected, and there is an increase in the mother's blood hormone levels,
concluding that multiple pregnancy is a greater demand for the woman's body and
contributes to the increase of complications such as: weight gain,
preeclampsia, among others (Mayo Clinic, 2022).
Fetal
complications are associated with prematurity and low birth weight since the
greater the number of fetuses, the shorter the duration of gestation and the
lower birth weight,
Some
of the complications include: evanescent twin syndrome, feto-fetal transfusion
syndrome, congenital defects, and growth retardation (Rodrigo, Aparicio
Caballero, & Salvador, 2022).
The
maternal-fetal dyad is a bond that is associated with emotional and cognitive
aspects that allow the fetus to be recreated as another human being. This bond
is expressed through health practices aimed at seeking the protection and
well-being of the fetus, and as a result of certain problems and complications
during pregnancy, such as multiple pregnancies and gestational hypertension,
among others, there is a risk of alteration of this bond (Alvarez Martinez,
2021).
For
this reason, the risk of maternal-fetal dyad disruption was chosen as the main
nursing diagnosis (DxEp).
Identification of Collaboration Problems (CPs) and their
Complication Risks (CRs)
To
determine of complication problems and complication risks, in relation to twin
pregnancy with preeclampsia, the Manual of Nursing Diagnoses manual Carpenito,
2017) was used.
Collaborative
Problem in the Prenatal Period: Gestational Hypertension The risks of
complication are:
CR
of malignant hypertension CR of convulsions
CR proteinuria
CR of fetal compromisse 32
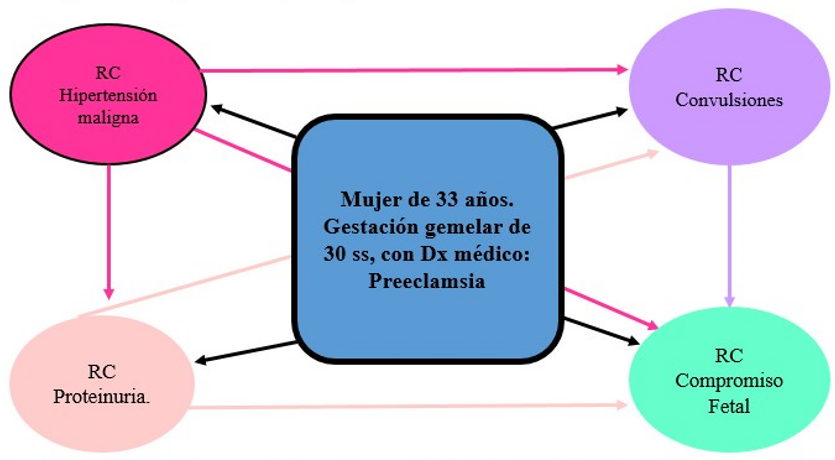
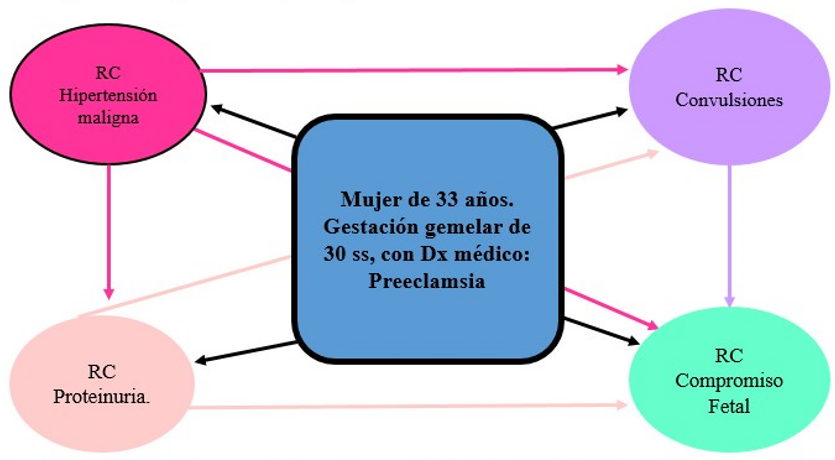
Figure 2.
Reasoning network based on the AREA Model for prioritization of major
complication risk
Identification of the main CR
Malignant
hypertension has been identified as the main complication risk (CR) because it
was the one with the highest ratio compared to the others, and it is linked to
CR seizures, CR proteinuria and CR fetal compromise.
CR
Malignant hypertension
Malignant
hypertension is very high blood pressure that appears suddenly and rapidly, and
is capable of triggering serious complications in the patient.
Justification
of the main CR
Malignant
hypertension is a type of hypertensive emergency and is so dangerous that it
can cause complications such as organ failure (Medical News Today, 2021).
McCarthy
(2022) defines malignant hypertension as an increase in blood pressure such an
extent that it causes organ damage, affecting the nervous system,
cardiovascular system and kidneys. He also states that prompt treatment can
prevent serious problems such as organ damage to the blood vessels, eyes,
heart, spleen, kidneys and brain.
The
nursing role in severe or malignant hypertension consists of providing absolute
rest to the patient, assessing blood pressure frequently, cardiac monitoring,
providing reassurance to the patient, and administering oxygen. If necessary,
perform an electrocardiogram, monitoring of vital functions, as indicated by
the physician, oncolysis, and extraction of analytical tests, and monitoring
for possible side effects of drug treatment such as hypotension, nausea,
vomiting, and headache. Observe the cardiac monitor for possible rhythm
disturbances or signs of myocardial ischemia. Constantly assess the state of
consciousness and observe the patient for signs of cerebral hemorrhage (Ybarra
Clemente & Marin Gasco, 2021).
In
conclusion, the clinical manifestation of the patient responds to the
symptomatology of malignant hypertension and the risk of suffering
multisystemic organ failure if she is not.
Timely
intervention should prevent, treat, and control the warning signs of
hypertension.
Planning of the main nursing diagnosis (DxEp)
After
performing the assessment and obtaining a nursing diagnosis, we proceed to make
a follow-up plan for the patient using the Nursing Outcomes Classification NOC
(Sue Moorhead et al., 2018) and Nursing Interventions Classification NIC
Butcher Howard et a., 2018).
(00209). Risk of
alteration of the maternal-fetal dyad evidenced by complications in pregnancy
due to multiple gestation.
Definition:
Vulnerable to disruption of the symbiotic relationship between mother and fetus
due to comorbidities or pregnancy-related conditions that may affect health.
NANDA-I Taxonomy, (Heather Herdman et al.,2021).
Domain
8: Sexuality
Class
3: Reproduction
NOC
results of the DxEp
According
to the NOC taxonomy, the following corresponds to the DxEp:
(0111).
Fetal status: Prenatal
Definition:
The degree to which fetal signs are within normal limits from conception to the
onset of labor.
Domain: Functional
health (1) Class: development and growth (B) (1902). Risk control.
Definition:
Personal actions to understand, avoid, eliminate or reduce modifiable health
threats.
Domain:
Health knowledge and behavior (IV) Class: Risk control and safety (T)
(1214).
Level of agitation.
Definition:
Severity of manifestations of physiological and behavioral disorders of stress
or biochemical triggers.
Domain:
Psychosocial health (III) Class: Psychological well-being (M)
(1302)
Coping with problems.
Definition:
Personal actions to control stressors that strain the individual's resources.
Domain: Psychosocial
health (III) Class: Psychosocial adaptation (N) DxEp NOC prioritization.
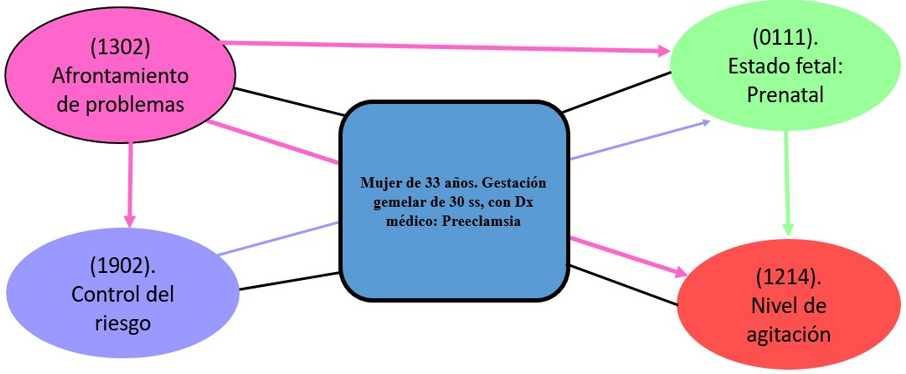
We
will perform the critical reasoning network analysis to define the main NOC
(figure 3).
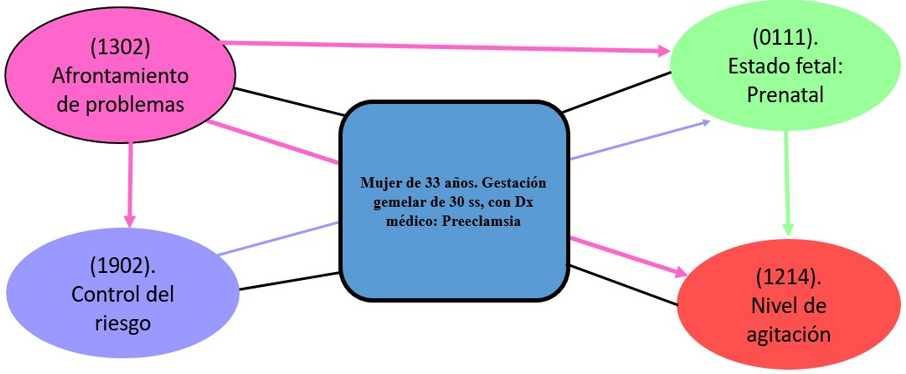
Figure 3.
Reasoning network based on the AREA Model for DxEP NOC prioritization
DxEp Main NOC Justification
NOC prioritized from
the DxEp
Coping
with problems: this is understood as the way in which the person manages losses
in bodily functions or disabilities resulting from illness (Navarro and Bueno
2015).
According
to Nola Pender, a nurse and author of the Health Promotion Model (HPM),
behavior is motivated by the desire to achieve happiness and human potential.
She is interested in creating a nursing model that provides answers about how
people make decisions about their own health care. Her goal is to illustrate
the multifaceted nature of people in their interactions with the environment as
they attempt to achieve a desired state of health; she emphasizes the
connection between personal characteristics and the experiences, knowledge,
beliefs, and situational aspects related to health behavior or behavior a
person wishes to achieve.
In
conclusion, it can be said that problem coping is the way in which the person
handles and/or accepts problems in order to achieve a solution.
(1302) Coping with
problems.
Definition:
Personal actions to control stressors that strain the individual's resources.
Domain:
Psychosocial health (III) Class: Psychosocial adaptation (N)
|
Table 1. Main
NOC score for DxEp
|
|
NOC
|
Initial Score
|
Diana Score
|
Weather
|
|
(1302) Coping with problems
|
2
|
4
|
12
|
In
relation to the score plotted for the main NOC measurement for the DxEp, the assessment
at the beginning of the nursing interventions was 2 points (Rarely
demonstrated), and after the administration of nursing care, a Target score of
4 points (Frequently demonstrated) is expected to be reached.
|
Table
2.
Main NOC indicator
|
|
Indicators
|
Initial Score
|
Diana Score
|
Weather
|
|
(130223) Obtains assistance from a healthcare
professional
|
2
|
4
|
12
|
|
(130205) Verbalize
acceptance of the situation
|
2
|
4
|
12
|
|
(130220) Seeks accredited information on the diagnosis
|
2
|
4
|
12
|
|
(130222)
Search Proven treatment information
|
2
|
4
|
12
|
Regarding
the indicators plotted for the main NOC measurement for the DxEp, the
assessment at the beginning of the nursing interventions was 2 points (Rarely
demonstrated), and after the administration of nursing care, a Target score of
4 points (Frequently demonstrated) is expected to be reached.
NIC interventions for the DxEp NOC
Nursing
interventions were identified, using the NIC nursing intervention
classification taxonomy Butcher Howard et al., 2018).
(5602) Teaching:
Disease Process.
Definition:
Helping the patient understand information related to a specific disease
process.
Domain:
3. Behavioral
Class:
S. Interventions to facilitate learning
Activities
·
(560201)
Review the patient's knowledge of his or her condition.
·
(560202)
Provide information about available diagnostic measures, as appropriate.
·
(560203)
Discuss therapy/treatment options.
·
(560204)
Instruct the patient which signs and symptoms to report to the health care professional,
as appropriate.
· (6610) Risk identification:
1.
Definition:
Analysis of potential risk factors, determination of health risks and
prioritization of risk reduction strategies for an individual or group of
people.
2.
Domain
4: Safety.
3.
Class
W. Risk control.
Activities
·
(661001)
Review medical history and previous documents to determine evidence of current
or previous medical and care diagnoses.
·
(661002)
Determine the availability and quality of resources (psychological, economic,
educational, family and other social resources, and community).
·
(661003)
Identify the center's resources to help reduce the risk factors for risk.
·
(661004)
Determine compliance with medical and nursing treatments.
· (5270) Emotional support:
1.
Definition:
Providing security, acceptance and encouragement in times of stress.
2.
Domain
4: Behavioral.
3.
Class
R: Coping assistance.
Activities
·
(527001)
Hugging or touching the patient to provide support.
·
(527002)
Help the patient recognize feelings such as anxiety, anger or sadness.
·
(527003)
Staying with the patient and providing feelings of security during periods of
heightened anxiety.
·
(527004)
Providing assistance in decision making.
With
respect to the planned interventions on: teaching of the disease process, identification
of risks and emotional support, provided to the patient in a 12-hour shift, the
planning was positive, with a noticeable improvement in the patient, thus
stabilization of her symptoms.
Major
Complication (CR) Risk Classification: Malignant Hypertension
After
performing the assessment and obtaining a nursing diagnosis, we proceed to make
a follow-up plan for the patient using the Nursing Outcomes Classification NOC
(Sue Moorhead et al.,2018) and Nursing Interventions Classification NIC (Butcher
Howard et al., 2018).
NOC
result of the main CR (RCp)
The
NOC taxonomy responds to the results we wish to achieve in the patient, using
4-digit codes and 6-digit indicators.
The
RCp Malignant hypertension, responds to the following NOCs: (1822) Knowledge:
maternal health in preconception (0401) Circulatory status.
(0405)
Cardiac tissue perfusion (2112) Severity of hypertension (0504) Renal function
(2112).
Severity
of hypertension (0504) Renal function 42.
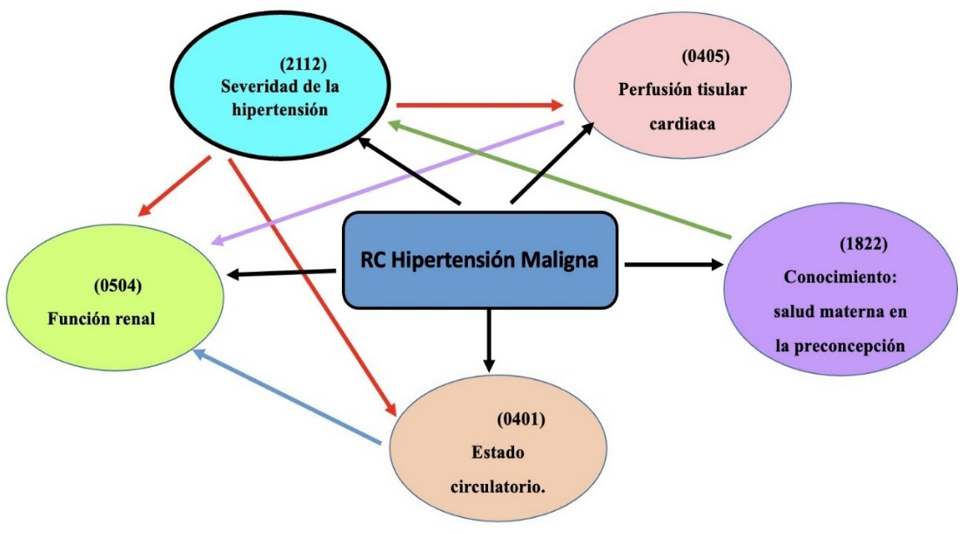
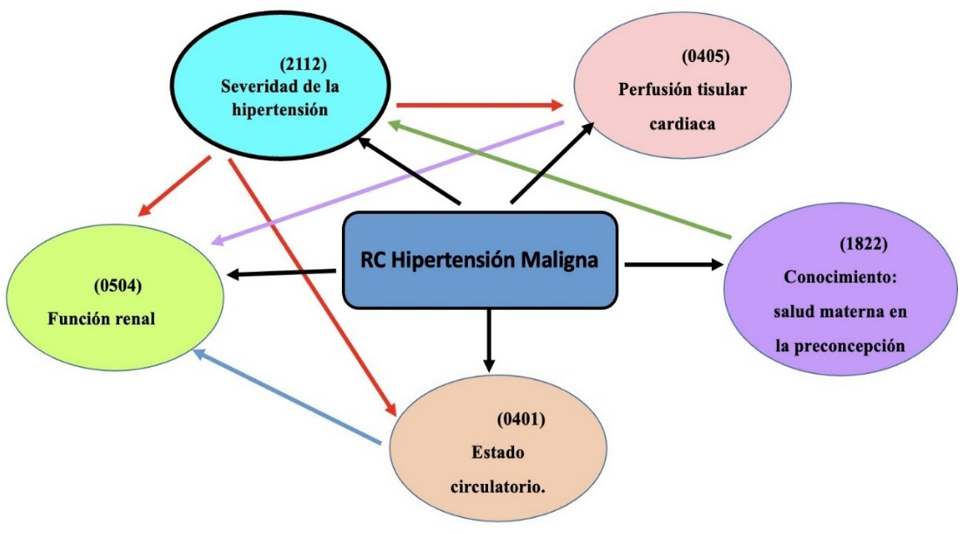
Figure 4.
Reasoning network based on the AREA Model for the prioritization of the NOC of
the main CR
Prioritized
NOC of the main CR Malignant Hypertension
(2112) Severity of hypertension
Definition:
"Severity of signs and symptoms due to chronic blood pressure."
(Moorhead et al., 2018)
Domain:
perceived health (V) Class: symptomatology (V)
|
Table 3.
Main NOC score of the main CR
|
|
NOC
|
Initial Score
|
Diana Score
|
|
(2112) Severity of hypertension
|
2
|
4
|
In
relation to the main NOC score of the RCp, according to the Likert scale, an
initial score of 2 points (substantial) was obtained for the patient's
assessment, with the goal of obtaining a target score of 4 points (Mild) after
nursing professional's interventions during a 12-hour shift, giving a positive
approach to the patient's evolution.
|
Table 4.
Scores of the main NOC indicators of the main
|
|
Indicators
|
Initial Score
|
Diana Score
|
Weather
|
|
(211207) Headache
|
2
|
4
|
12
|
|
(211212) Tinnitus
|
2
|
4
|
12
|
|
(211216) Increased systolic P/A.
|
2
|
4
|
12
|
|
(211217) Increase in diastolic P/A
|
2
|
4
|
12
|
Interventions
for risk of major complication (RCp)
Nursing
interventions were considered in relation to RCp: Malignant hypertension, for which
we used the NIC nursing intervention classification taxonomy Butcher Howard et
al., 2018).
(6200) Emergency care
Definition:
"Perform assessment and implement therapeutic measures in urgent
situations" (Butcher et. al., 2018).
Field
4: safety: supportive care against damage Class U: crisis control.
Activities
(620001)
Activate medical emergency system (620002) Monitor vital signs of hypertension
(620001) Activate medical emergency system (620002) Monitor hypertension vital
signs
(620003)
Providing safety and emotional support to the patient.
(620004)
Assist with treatment by providing information about the potential situation.
(6771)
Electronic fetal monitoring: antepartum.
·
Definition: "Electronic assessment of fetal
cardiac response to movement, external stimuli, or uterine contractions during
antepartum testing" Butcher et. al., 2018).
·
Field
5: Family
·
Class
W: Caring a new baby
Activities
(677101)
Review obstetrical history, if available, to determine obstetrical or medical
risk factors concerning fetal status that require pre-delivery testing for
fetal status.
(677102)
Verify fetal and maternal heart rate before initiating electronic fetal
monitoring.
(677103)
Interpret the electronic monitoring strip for long-term fetal heart rate
variability and presence of accelerations, decelerations or spontaneous
contractions.
(677104)
Observe the monitoring strip for the presence or absence of late decelerations.
(677105)
Communicate test to the responsible physician or midwife.
(4062) Circulatory care, arterial insufficiency
Definition:
"Improvement of arterial circulation" Butcher et. al., 2018).
Field
2: Complex physiological: Care that supports homeostatic regulation Class N:
Control of tissue perfusion.
Activities
(406201)
Perform comprehensive assessment of peripheral circulation edema, capillary
refill, color and temperature.
(406202)
Evaluate edema and peripheral pulses (406203) Monitor water balance.
This
last intervention was chosen, since the main complication risk is "malignant
hypertension", through the intervention of seizure management; being the
drug used magnesium sulfate parenterally, executed in emergency care; thus
avoiding the compromise of fetal distress.
Execution
To
apply the nursing interventions and activities, a 12-hour day shift is chosen;
for this, the NIC Nursing Intervention Classification book was used Butcher et.
al., 2018).
|
Table
5.
Timeline of interventions/nursing activities in risk of maternal-fetal dyad
disruption
|
|
Date
|
Interdependent
and dependent activities
|
Shifts
|
|
8:30
|
10:00
|
12:00
|
14:00
|
16:00
|
18:00
|
20:30
|
|
9/9/2022
|
(00209) Risk of
alteration of the maternal-fetal dyad
|
X
|
|
|
|
|
|
|
|
|
Activities:
|
|
|
|
|
|
|
|
|
|
Teaching: Disease
Process.
|
X
|
X
|
|
|
|
|
|
|
|
Review the patient's knowledge
of his or her condition.
|
X
|
X
|
|
|
|
|
|
|
|
Provide information
about diagnostic measures
|
|
X
|
X
|
|
|
|
|
|
|
available, as
appropriate.
|
|
|
X
|
X
|
|
|
|
|
|
Discuss
therapy/treatment options.
|
|
|
|
X
|
X
|
|
|
|
|
Instruct the patient
on what signs and symptoms he/she should be aware of.
|
X
|
|
|
|
|
|
|
|
|
notify the health
care professional, as appropriate.
|
X
|
|
|
|
|
|
|
|
|
Risk identification.
|
X
|
|
|
|
|
|
|
|
|
Review medical
history and previous documents for
|
X
|
X
|
|
|
|
|
|
|
|
determine evidence of
current or past medical and care diagnoses.
|
|
X
|
X
|
|
|
|
|
|
|
Determine the
availability and quality of resources (psychological, economic, educational,
family and other social resources; and
|
X
|
X
|
X
|
X
|
X
|
X
|
X
|
|
|
community).
|
X
|
|
|
|
|
|
|
|
|
Identify the center's
resources to help reduce the risk factors that may cause the
|
X
|
X
|
|
|
|
|
|
|
|
risk.
|
X
|
|
|
X
|
|
|
|
|
|
Determine compliance
with medical and medical treatments
|
|
|
X
|
|
|
|
|
|
9/9/2022
|
Nursing.
|
|
|
|
|
|
|
|
|
|
Emotional support
|
|
|
|
|
|
|
|
|
|
Hug or touch the
patient to provide support.
|
X
|
|
|
|
|
|
|
|
|
Helping the patient
to recognize feelings such as anxiety, anger
|
X
|
|
|
|
|
|
|
|
|
or sadness.
|
X
|
|
X
|
|
X
|
|
X
|
|
|
Staying with the
patient and providing feelings of safety and security
|
X
|
X
|
X
|
X
|
X
|
X
|
X
|
|
|
during periods of
high anxiety.
|
X
|
|
|
|
|
|
|
|
|
Provide assistance in
decision making.
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
|
|
(RCp) Malignant
hypertension
|
x
|
|
|
|
|
|
|
|
|
Activities:
|
X
|
X
|
X
|
X
|
X
|
X
|
X
|
|
|
Emergency care
|
X
|
X
|
X
|
X
|
X
|
X
|
X
|
|
|
Activate the medical
emergency system.
|
X
|
X
|
X
|
X
|
X
|
X
|
X
|
|
|
Monitor vital signs
for hypertension.
|
X
|
X
|
X
|
X
|
X
|
X
|
X
|
|
|
Provide security and
emotional support to the patient.
|
X
|
|
X
|
|
X
|
|
|
|
|
Assist with treatment
by providing information about the situation.
|
X
|
|
X
|
|
X
|
|
|
|
|
Electronic fetal
monitoring: before delivery
|
X
|
|
X
|
|
X
|
|
|
|
|
Review obstetrical
history, if available, to determine obstetrical or medical risk factors
concerning fetal status that require pre-delivery testing to ascertain the
|
X
|
|
|
X
|
|
|
X
|
After
administration of the main nursing interventions, in response to the DxEp NOC
and the RCp NOC, change scores of +1 and +2 were obtained.
Evaluation
It
was performed based on the assessment of the pregnant woman's condition at
admission, compared with the results the administration of the nursing
interventions.
A
follow-up period was established in the gynecology hospitalization service in
the day shift; some progress was observed, however, continued care was needed.
Nursing activities were evaluated based on the comparison of the patient's
health status and the effectiveness of the planned outcomes.
Evaluation
of the Outcome of the main Dx. E. main
(00209). Risk of alteration of the maternal-fetal
dyad
Evidenced by
complications in pregnancy due to multiple gestation.
Definition:
Susceptible to disruption of the symbiotic mother-fetal relationship as a
result of comorbid or pregnancy-related conditions that may health.
Domain
8: Sexuality.
Class
3: Reproduction.
|
Table
6. Scores
of the main diagnostic indicators
|
|
Indicators
|
Initial Score
|
Diana Score
|
Score achieved
|
Weather
|
|
(130223)
Obtains assistance from a health professional
|
2
|
4
|
3
|
12
|
|
(130205)
Verbalizes acceptance of the situation
|
2
|
4
|
3
|
12
|
|
(130220)
Search for information accredited on the diagnosis
|
2
|
4
|
3
|
12
|
|
(130222)
Search Information accredited on the treatment
|
2
|
4
|
3
|
12
|
Analyzing
the results obtained, the following is observed in relation to the indicators table
6; represented: (130223) Obtains help from a health professional, (130205)
Verbalizes acceptance of the situation, (130220) Seeks accredited Information
about the diagnosis, (130222) Seeks accredited Information about the treatment,
the patient started with a score of 2 (Rarely demonstrated) and reached a score
of 3 (Sometimes demonstrated) in a period of 12 hours, During this time she was
able to be attended by a multidisciplinary team, where she was able to
verbalize her situation that affected her, and was able to find a diagnosis of
her disease process and obtain an adequate treatment to stabilize her altered
health patterns and achieve the recovery of the mother and the preservation of
the pregnancy through the care applied.
(1302)
Coping with problems
Definition:
Personal actions to control stressors that strain the individual's resources.
Domain:
Psychosocial health (III) Class: Psychosocial adaptation (N)
|
Table
7.
Main NOC score for DxEp
|
|
NOC
|
Initial Score
|
Diana Score
|
Score achieved
|
Weather
|
|
(1302)
Coping with problems
|
2
|
5
|
4
|
12
|
The
interventions have been carried out achieving the proposed target score, being
the initial score of 2 points, after a period of 12 hours of permanence in the
service of gynecology hospitalization. A score of 4 points according to the
Likert scale was achieved, reaching compliance with problem coping assessment
of major complication risk outcome.
|
Table 8. Main
NOC score of the main CR
|
|
NOC
|
Initial Score
|
Diana Score
|
Score Achieved
|
|
(2112)
Severity of hypertension
|
2
|
5
|
4
|
The
programmed nursing interventions were carried out, obtaining the proposed
target score, the initial score being 2 points, after a period of 12 hours in
the hospital. A score of 3 points was achieved according to the Likert scale,
achieving moderate management of the severity of hypertension in the pregnant
woman.
Table
9. Scoring of the main NOC indicators of the main CR
|
|
Indicators
|
Initial Score
|
Diana Score
|
Score achieved
|
Weather
|
|
(211207)
Headache
|
2
|
5
|
4
|
12
|
|
(211212)
Tinnitus
|
2
|
5
|
4
|
12
|
|
(211216)
Increased systolic P/A.
|
2
|
5
|
4
|
12
|
|
(211217)
Increase in diastolic P/A
|
2
|
5
|
4
|
12
|
Observing
the results obtained, the following is observed: in relation to the indicators
in table 9, represented: (21207) headache, (211212) tinnitus, (211216) increase
in systolic P/A, (211217) increase in diastolic P/A, the patient started with a
score of 2 (substantial) and a score of 4 (mild) on the Likert scale in a
period of 12 hours, achieving a good score in the stabilization of the
symptomatology presented through the care applied by the multidisciplinary
health team.
DISCUSSION
The
patient in the present study was admitted to the gynecology hospitalization
service, presenting a temperature of 38,7 °C, headache, tinnitus,
abdominopelvic pain, lower limb edema, and P/A 190/110mm Hg, with medical
diagnosis: preeclampsia and twin gestation of 30 weeks due to FUR and CR of
malignant hypertension as a consequence of the disorder in the third trimester
of pregnancy; for which, she is in the gynecology hospitalization service after
being referred from the emergency area for timely care to avoid damage.
After
reviewing the literature, numerous studies have shown that nursing care is
essential, comprehensive, and of high quality and is key to preventing
cerebrovascular, cardiovascular, and renal diseases. In affirming the above,
there is scientific evidence that the nursing professional has a key role in
prenatal care for the timely detection, prevention, diagnosis, and treatment
that can attenuate the factors that can condition maternal and perinatal
morbidity and mortality. (Guarnizo et. al., 2019).
The
elaboration and execution of the nursing care plan as an instrument to
establish and document the actual situation of the patient, the expected
outcomes, interventions, and evaluation allow constant monitoring to improve
the weaknesses found. Nursing care is both autonomous and collaborative for the
delivery of service care (PAHO, 2022).
Psychophysiological
changes during pregnancy are often accompanied by different emotions, which
occur throughout pregnancy, such as mood swings, irritability, fear, and
anxiety. For this reason, a pregnant woman is considered emotionally unstable. She
needs to be treated humanely and feel satisfied with her care by a qualified
multidisciplinary team of medical professionals. Likewise, we consider the
mother's family as another major component of the comprehensive care provided
and of the nursing intervention that should be directed to the partner and
family, who are also directly concerned with maternal health problems. To help
improve (Maset, 2021).
In
the case presented, the informant was the patient; data collection and
assessment were carried out through assessment instruments, relying on
interviews and observation, as well as other sources of data collection.
Nursing
interventions are based on the theories of Hildegard E. Peplau who seeks to
highlight the psychological tasks that develop from the nurse-patient
relationship, depending on the nurse's ability to recognize the difficulties
posed by relationships with their patients and the ability to help them resolve
their difficulties, so that they can develop new faculties for coping with
problems (Martinez Esquivel, 2020).
This
theory, in relation to the patient's situation after the diagnosis of Risk of
alteration of the maternal-fetal dyad in the patient with twin gestation of 30
weeks, guided us to improve the coping of problems by improving the
nurse-patient relationship. Likewise, our care was oriented in the theory of
"Humanized Care" by Jean Watson, reducing the risk of dehumanization
in patient care and rescuing the human, spiritual, and transpersonal aspects
during nursing care of the pregnant patient (Gaona Castillo, 2021).
The
Risk of alteration of the maternal-fetal dyad occurs as a consequence of
pregnancy complications such as hypertension and due to a deficit of knowledge
on the part of the mother, in the face of which the nursing professional
participates in the timely treatment, avoiding the occurrence of maternal
vascular lesions, such as compromised hepatic, renal damage, and consequently
fetal compromise (Department of Obstetrics, UC of Chile, 2020).
Malignant
hypertensive CR manifests with a high risk of seizures and Risk of fetal
compromise (Tango, 2020). Timely intervention with the actions of Nursing plays
a very important role in the prevention of this problem of maternal and
perinatal complications, with the aim of contributing to the reduction of
maternal morbidity and establishing technical criteria for the prevention, diagnosis,
treatment, and control of preeclampsia.
To
conclude, as health professionals, we have the responsibility to perform a good
assessment and, through our timely care, reduce the risks of complications in
the maternal-fetal binomial. After the nursing care provided to the patient at
a critical moment, we were able to assess a favorable evolution compared to the
initial phase of care in the gynecology hospitalization service.
Limitations
The
limitations encountered in the development of the case study in the twin
pregnancy with preeclampsia were:
Limited
time for monitoring and care who was only seen during a 12-hour shift in the
gynecology service.
Care
could not be continued in the following days, due to interference with the
working hours of nursing professionals.
When
applying nursing care, we had the limitation of finding the appropriate
diagnoses and interventions for the patient's pathology because the NOC and NIC
did not include the diagnosis of preeclampsia.
At
the same time, due to the COVID-19 pandemic situation, the conditions for
family access to information were limited since visits were restricted in the
institution.
CONCLUSIONS
Preeclampsia
is a hypertensive disorder that can occur during pregnancy from 20 weeks of gestation,
and becomes a serious condition representing a major danger to the mother-fetus
binomial. In Peru (2020-2021), maternal deaths represent 21,4 % (2020) and 15,8
% (2021). (MINSA, 2022), this indicator allows measuring the impact of health
policy on the provision of maternal health services.
The
PAE was applied, developing the nursing care plan, according to the NANDA I.
taxonomy, NOC, NIC, and Lynda Carpenito's bifocal model for a patient with twin
gestation, preeclampsia and risk of complication: malignant hypertension, in
order to promote professional practice with a creative approach based on human
responses specific situations.
The
assessment by functional patterns was based on the theoretical framework, on
the nursing theory of Hildegard Peplau and Jean Watson, which helped to
identify the nursing diagnosis of risk of alteration of the maternal-fetal dyad
and the problem of collaboration in the prenatal stage, gestational
hypertension and risk of complication of malignant hypertension.
The
risk factors of the patient with twin gestation and preeclampsia were
identified and described, considering situations, personal characteristics, and
diseases that have hindered the patient's ability to continue with the
pregnancy and project us toward recovery due to her vulnerability to the risk
of complication: malignant hypertension.
90
% of the activities of the nursing care plan were fulfilled, where the actions
were protocolized based on the patient's needs, monitored to consolidate the
evaluation and define the improvement of the interventions in the patient
through participatory work with the multidisciplinary team for the solution of
the collaborative problem.
Nursing
care, as a basic and primordial tool, strengthened the autonomy and empowerment
of the nurse in the care of the patient with preeclampsia, achieving the
objectives in the evolution of the disease process.
Through
the care plan, the proposed objectives were achieved by prioritizing the main
nursing diagnosis to provide timely and quality care, improving maternal and
fetal health.
BIBLIOGRAPHIC REFERENCES
1. Blanco Balbeito, Nubia, & Betancourt Roque,
Yovana. (2021). La enfermería: ciencia constituida. Revista Eugenio Espejo,
15(2), 3-5. https://doi.org/10.37135/ee.04.11.02
2. Alvarez Fernandez, I., Prieto, B., & Alvarez,
F. V. (2018). Preeclampsia. Revista Del Laboratorio Clínico, 81-89.
3. Alvarez Martinez, E. (Septiembre de 2021). El
apego desde el útero. Obtenido de Psicociencias Org: https://www.psicociencias.org/pdf_noticias/El_apego_desde_el_utero_E.Alvarez.pdf
4. Amaro Cano, M. D. (Abril de 2004). SCIELO.
Obtenido de Revista Cubana de Enfermería: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0864-03192004000100010
5.
Ascarelli, M. H., Johnson, V., May, W. L., & Martin, J. N. (2005).
Postpartum preeclampsia management with furosemide: a randomized clinical
trial. Obtenido de Epistemonikos Foundation: https://www.epistemonikos.org/es/documents/11bdff530f72fb830b7c5ec7b01a7288dcdb647b#:~:text=La%20terapia%20breve%20furosemida%20despu%C3%A9s,la%20necesidad%20de%20terapia%20antihipertensiva.
6. Bravo Andrés, N., Ledesma Redrado, A., Maestro
Cebamanos, S., & Delgado Roche, E. (2021). Plan de cuidados de enfermería
en la preeclampsia. A propósito de un caso. Fundación Dialnet .
7.
Bulechek, G. M., Butcher, H. K., Dochterman, J. M., & Wagner, C. M. (2014).
Clasificación de Intervenciones de Enfermería (NIC)
Sexta edición. Barcelona: Elsevier.
8. Carpenito, L. J. (2017). Manual de Diagnósticos
Enfermeros (15.edición ed.). Philadelphia, Estados Unidos: Wolters Kluwer.
9. Carvajal Carvajal, C. (Diciembre de 2017).
SCIELO. Obtenido de Medicina Legal de Costa Rica: https://www.scielo.sa.cr/scielo.php?script=sci_arttext&pid=S1409-00152017000200090
10. Centro Nacional de Epidemiología, Prevención y
Control de Enfermedades. (2018). VOLUMEN 27 - SE 44-2018 Semana epidemiológica
(del 28 de octubre al 03 de noviembre de 2018). Lima: Boletín Epidemiólogico
del Perú.
11. Chavez Lopez, S. I., & Ñahuin Huaroc, Y. K.
(2018). Tratamiento aplicado a gestantes con trastorno hipertensivo del
embarazo . Obtenido de Repositorio de Tesis Universidad Nacional de
Huancavelica: https://apirepositorio.unh.edu.pe/server/api/core/bitstreams/202b1c35-0974-45e0-9aef-099c25187c25/content
12.
Chimbo Oyaque, C. E., Mariño Tapia, M. E., Chimbo Oyaque, T. A., & Caicedo
Torres, C. E. (2018). Factores de riesgo y
predictores de preeclampsia: una mirada al futuro. Revista Latinoamericana de
Hipertensión. Clinica Delgado. (2019). Hipertensión arterial primaria
(Tratamiento farmacológico en grupos de pacientes y circunstancias
especiales). Lima. Obtenido de Auna Clínica
Delgado: https://clinicadelgado.pe/wp-content/uploads/2020/02/HAPpacientesespeciales.pdf
13. De Jesus Garcia, A., Jimenez Baez, M. V.,
Gonzales Ortiz, D. G., De La Cruz Toledo, P., Sandoval Jurado, L., & Kuc
Peña, L. M. (2019). Características clínicas, epidemiológicas y riesgo obstétrico
de pacientes con preeclampsia-eclampsia. Cancún,
México: Instituto
Mexicano del Seguro Social.
14. De La Puente Vaca, L. (2021). Importancia de los
cuidados de enfermería en la preeclampsia. Obtenido de Universidad de
Valladolid: https://uvadoc.uva.es/bitstream/handle/10324/47845/TFG-H2282.pdf;jsessionid=FCEB058DBF551027A94847F8012B062E?sequence=1
15. Departamento de Obstetricia de la UC de Chile.
(Octubre de 2020). Obstetricia Pautas de manejo. Obtenido de Facultad de
Medicina de la UC Chile: https://medicina.uc.cl/wp-
content/uploads/2020/10/pautas-de-manejo-obstetricia-uc.pdf
16. Diaz Cobos, D., Laparte, C., Ruiz-Zambrana, A.,
& Alcazar, J. L. (2015). Screening de primer trimestre de preeclampsia
tardía en gestantes de bajo riesgo en un centro de bajo volumen obstétrico:
validación externa de un modelo predictivo. Obtenido de Scielo: https://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1137-66272015000300003
17. Elers Mastrapa, Y., & Gilbert Lamadrid, M.
D. (2016). Relación enfermera-paciente: una perspectiva desde las teorías de
las relaciones interpersonales. Revista cubana de enfermería.
18. Gaona Castillo, J. A. (2021). Manejos de
enfermería en pacientes con preeclampsia: Revisión Sistemática. Ocronos.
19. Garcia Hermida, M. I., Garcia Remirez, C. G.,
& Garcia Rios, C. A. (2020). Comportamiento clínico epidemiológico de
gestantes adolescentes con hipertensión arterial. Archivo Médico Camagüey,
525-537.
20. Garcia Lopez, N. (19 de Mayo de 2020). Revista
electrónica de portales médicos. Obtenido de Plan de cuidados enfermeros en
paciente embarazada con hipertensión: https://www.revista-portalesmedicos.com/revista-medica/plan-de-cuidados-enfermeros-
en-paciente-embarazada-con-hipertension/
21. Gil Cipiran, F. (6 de Abril de 2021). Situación
epidemiológica de mortalidad materna en el Perú. Obtenido de Centro Nacional de
Epidemiología, Prevención y control de Enfermedades: https://www.mesadeconcertacion.org.pe/storage/documentos/2021-05-07/anexo-2-cdc-
minsa-muerte-materna-2020-2021-08-abril.pdf
22. Gomez Carbajal, L. M. (29 de Octubre de 2014).
SCIELO. Obtenido de Revista Peruana de Ginecología y Obstetricia: http://www.scielo.org.pe/scielo.php?script=sci_serial&pid=2304-5132&lng=es&nrm=iso
23. Gonzales Navarro, P., Martinez Salazar, G. G.,
Garcia Najera, O., & Sandoval Ayala, O. I. (2015). Preeclampsia, eclampsia
y HELLP . Revista Mexicana de Anestesiología, 118- 127. Grupo Inter-Agencial
para la estimación de la Mortalidad Materna de las Naciones Unidas. (Diciembre
de 2017). Panorama de la Situación de la Morbilidad y Mortalidad Maternas:
América Latina y el Caribe . Obtenido de Grupo de trabajo regional para la
reducción de la mortalidad materna: https://lac.unfpa.org/sites/default/files/pub-pdf/MSH-GTR-Report-
Esp.pdf
24. Guarnizo Tole, Mildred; Olmedillas Fernandez,
Hugo; Vicente Rodriguez, German. (16 de Enero de 2019). Revista cubana de
obstetricia y ginecología. Obtenido de Prácticas en enfermería para prevenir la
mortalidad materna de la mujer en edad fértil: https://revginecobstetricia.sld.cu/index.php/gin/article/view/381/299
25. Guevara Ríos, E. (2019). La preeclampsia,
problema de salud pública. Lima, Perú: Revista Peruana de investigación Materno
Perinatal.
26. Guevara Rios, E., & Meza Santibañez, L.
(2014). Manejo de la preeclampsia/eclampsia en el Perú. Revista Peruana de
Ginecología y obstetricia.
27. Juarez Rodriguez, P. A., & Garcia Campos, M.
D. (2009). La Importancia del cuidados de Enfermería. Revista Mexicana de
enfermería.
28. Lacunza Paredes, R. O., & Avalos Gomez, J.
(2019). ANTI-ANGIOGENESIS EN LA FISIOPATOLOGÍA DE LA PREECLAMPSIA. ¿LA PIEDRA
ANGULAR? . Revista Peruana de Investigación Matenro Perinatal.
29. Martinez Esquivel, D. (2020). Av Enferm.
Obtenido de Abordaje de enfermería basado en el modelo de Peplau sobre el
control de impulsos ineficaz: https://doi.org/10.15446/av.enferm.v38n1.80576
30. Maset, J. (22 de Diciembre de 2021). Cambios
físicos y psicológicos durante el embarazo.Obtenido de Cinfasalud: https://cinfasalud.cinfa.com/p/cambios-fisicos-y-psicologicos-
durante-el-embarazo/
31. Mayo Clinic. (11 de Junio de 2022). Mayo Clinic.
Obtenido de Preclampsia: https://www.mayoclinic.org/es-es/diseases-conditions/preeclampsia/symptoms-
causes/syc-20355745
32. Mayo Clinic. (25 de Enero de 2022). Mayo Clinic
Org. Obtenido de Embarazo de gemelos: Qué implican los embarazos gemelares o
múltiples para las madres: https://www.mayoclinic.org/es-es/healthy-lifestyle/pregnancy-week-by-week/in-
depth/twin-pregnancy/art-20048161
33. McCarthy, A. A. (2022). Hipertensión maligna
(emergencia hipertensiva, crisis hipertensiva, urgencia hipertensiva). Obtenido
de Western New York Urology Associates: https://www.wnyurology.com/content.aspx?chunkiid=629512
34. Medical News Today. (29 de Junio de 2021).
Emergencia hipertensiva: Causas, síntomas y tratamiento. Obtenido de Medical
News Today: https://www.medicalnewstoday.com/articles/es/hipertension-maligna
35. Mejia, R., & Sarto, A. (1996). https://www.medicinabuenosaires.com/revistas/vol56-96/3/preeclampsia.htm.
Medicina Buenos Aires. Obtenido de FISIOPATOLOGIA DE LA PREECLAMPSIA.
36. Melgarejo Aranda, H. N. (2021). Factores de
riesgos sociodemográficos y gineco obstétricos que influyen en la preeclampsia
en gestantes de un hospital público de Chancay, 2021. Obtenido de Repositorio
de Tesis Universidad Peruana Union: https://repositorio.upeu.edu.pe/bitstream/handle/20.500.12840/4485/Hilda_Trabajo_Especialidad_2021.pdf?sequence=1&isAllowed=y
37. Mena Tudela, D., Gonzales Chorda, V. M., Cervera
Gasch, A., Salas Medina, P., & Orts Cortes,. M. I. (2016). Cuidados Básicos
de Enfermería. Unión de Editoriales Universitarias Españolas.
38.
Moorhead, S., Johnson, M., Maas, M. L., & Swanson, E. (2014). Clssificación
de Resultados de enfermería (NOC) Medición de Resultados en Salud Quinta
edición. Barcelona: Elsevier.
39. Morales Garcia, B., Moya Toneut, C., Blanco
Balbeito, N., Moya Arechavaleta, N., Moya Arechavaleta, A., & Moya Toneut,
R. (29 de Septiembre de 2017). Infomed. Obtenido de Revista Cubana de
onstetricia y Ginecología: http://www.revginecobstetricia.sld.cu/index.php/gin/article/view/207/166
40. NANDA INTERNACIONAL. (2021-2023). Diagnósticos
Enfermería. Definiciones y clasificación Duodécima edición. Nueva York: Thieme.
(Heather Herdman et al.,2021)
41. OMS. (2013). Recomendaciones de la OMS para la
prevención y tratamiento de la preeclampsia y eclampsia. Obtenido de Who.org: https://apps.who.int/iris/bitstream/handle/10665/119742/WHO_RHR_14.17_spa.pdf
42. OPS. (1 de Agosto de 2019). Día de Concientización
sobre la Preeclampsia. Obtenido de Organización Panamericana de la Salud: https://www.paho.org/es/noticias/1-8-2019-dia-concientizacion-sobre-preeclampsia
43. OPS. (12 de Mayo de 2022). Día Internacional de
las Enfermeras y los Enfermeros. 12 de Mayo del 2022. Obtenido de paho.org: http://www.paho.org/es/campanas/dia-internacional-
enfermeras-enfermeros-12-mayo-2022
44.
Pereira Calvo, J., Pereira Rodriguez, Y., & Quiros Figueroa, L. (Enero de
2020). Revista médica Sinergia. Obtenido de
Actualización en preclampsia: https://revistamedicasinergia.com/index.php/rms/article/view/340/708
45.
Pesut , D., & Herman, J. (1999). Clinical Reasoning: The Art and Science of
Critical and Creative Thinking 1st Edición. Cengage
Learning.
46. Plasencia Nuñez, A. C. (2013). Universidad
Nacional de Trujillo. Obtenido de Repositorio: https://dspace.unitru.edu.pe/bitstream/handle/UNITRU/304/PlasenciaNuñez_A.pdf?sequence=1&isAllowed=y
47. Preeclampsia Fundation. (14 de Diciembre de
2021). preclampsia.org. Obtenido de Preeclampsia Fundation: https://www.preeclampsia.org/signos-y-sintomas
48. Rodrigo, A., Aparicio Caballero, M., &
Salvador, Z. (2022). Riesgos del embarazo múltiple para la madre y los bebés.
Reproducción Asistida ORG. Obtenido de Reproducción Asistid ORG: https://www.reproduccionasistida.org/riesgos-del-embarazo-multiple/
49. Romero E., M. A., Vargas H., V. M., & Acosta
A., G. (2012). La preeclampsia es un problema de salud pública mundial.
Santiago, Chile: Revista chilena de obstetricia y ginecología.
50. Salas Ramirez, B., Montero Brenes, F., &
Alfaro Murillo, G. (2020). Trastornos hipertensivos del embarazo. Revista
Médica Sinergia.
51. Segovia Vásquez, M. R., & Álvarez, C.
(Diciembre de 2018). Criterios de severidad de la enfermedad hipertensiva del
embarazo. Obtenido de Revista Nacional (Itauguá) - SCIELO: http://scielo.iics.una.py/scielo.php?script=sci_arttext&pid=S2072-81742018000200105
52.
Stanford Medicine. (2022). Stanford Medicine Childrens Health. Obtenido
de Complicaciones de un embarazo múltiple: https://www.stanfordchildrens.org/es/topic/default?id=complicationsofmultiplepregnancy-85-P08045
53. T. Dulay, A. (18 de Octubre de 2020). MSD.
Obtenido de Manual MSD: https://www.msdmanuals.com/es-pe/professional/ginecolog%C3%ADa-y-obstetricia/anomal%C3%ADas-del-embarazo/preeclampsia-y-eclampsia
54. Tacuri Alcívar, A. J., Rodríguez Gómez, K. E.,
Cuadro Ayala, M. L., & Ramírez Moran, E. R. (2022). Factores clínicos y
quirúrgicos que influyen en la indicación de cesárea en. Revista
Científica Dominio de las ciencias, 1600-1616.
55.
Vasconselos Amorim, T., De Oliveira Souza, I. E., Vasconselos Moura, M. A.,
Acevedo Queiroz, A. B., & Oliveira Salimena, A. M. (2017). Perspectivas
de los cuidados de enfermería en el embrazo de alto riesgo: revisión
integradora. Enfermería Global.
56. Velumani, V., Duran Cardenas, C., &
Hernandez Gutierrez, L. (2022). Revista de Facultad de Medicina de Mexico.
Obtenido de Preeclampsia: una mirada a una enfermedad mortal: https://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S0026-17422021000500007
57. Ybarra Clemente, H., & Marin Gasco, V. (22
de Marzo de 2021). Cuidados de enfermería en el paciente con hipertensión
arterial. Obtenido de Zona Hospitalaria: https://zonahospitalaria.com/cuidados-de-enfermeria-en-el-paciente-con-hipertension-arterial/
58. Villarreal-Ríos, Enrique, Camacho-Álvarez, Iraís
Anahury, Vargas-Daza, Emma Rosa, Galicia Rodríguez, Liliana, Martínez-González,
Lidia, & Escorcia Reyes, Verónica. (2020). Antecedente heredofamiliar de
hipertensión (padre-madre), factor de riesgo para familia hipertensa (hijos).
Revista Clínica de Medicina de Familia, 13(1), 15-21. Epub 20 de abril de 2020.
Recuperado en 14 de julio de 2023, de http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1699-695X2020000100004&lng=es&tlng=es.
59.
Rojas Pérez, Lino Arturo, Villagómez Vega, María Daniela, Rojas Cruz, Augusto
Ernesto, & Rojas Cruz, Andrés Eduardo. (2019).
Preeclampsia - eclampsia diagnóstico y tratamiento. Revista Eugenio Espejo ,
13(2), 79-91. https://doi.org/10.37135/ee.004.07.09
60. Calderón Restrepo, Nevardo, Pérez Muñoz,
Ánderson, Gutiérrez Marín, Jorge Hernán, Sanín Blair, José Enrique, García
Posada, Raúl A., Cuesta, Diana Paola, & Campo Campo, María Nazareth.
(2022). Manejo expectante en preeclampsia severa remota del término (24-33,6
semanas): experiencia en centro de alta complejidad. CES Medicina, 36(3),
38-51. Epub January 20, 2023. https://doi.org/10.21615/cesmedicina.6881.
61. Checya-Segura, Jorge, &
Moquillaza-Alcántara, Víctor Hugo. (2019). Factores asociados con preeclampsia
severa en pacientes atendidas en dos hospitales de Huánuco, Perú.
62. Ginecología y obstetricia de México, 87(5),
295-301. Epub 30 de junio de 2021. https://doi.org/10.24245/gom.v87i5.2753
63.
Rojas Pérez, Lino Arturo, Villagómez Vega, María Daniela, Rojas Cruz, Augusto
Ernesto, & Rojas Cruz, Andrés Eduardo. (2019).
Preeclampsia - eclampsia diagnóstico y tratamiento. Revista Eugenio Espejo ,
13(2), 79-91. https://doi.org/10.37135/ee.004.07.09
FINANCING
The
authors received no funding for the development of this research.
CONFLICT OF INTEREST
The
authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization:
Salazar A Josselyn-Andrea, Salcedo Victcely-Del Carmen, Sofia D.
Vivanco-Hilario, Wilter C. Morales-Garcia.
Data
curation: Salazar A Josselyn-Andrea, Salcedo Victcely-Del
Carmen, Sofía D. Vivanco-Hilario, Wilter C. Morales-García.
Formal analysis:
Salazar A Josselyn-Andrea, Salcedo Victcely-Del Carmen, Sofía D.
Vivanco-Hilario, Wilter C. Morales-García.
Research: Salazar A
Josselyn-Andrea, Salcedo Victcely-Del Carmen, Sofia D. Vivanco-Hilario, Wilter
C. Morales-Garcia.
Methodology:
Salazar A Josselyn-Andrea, Salcedo Victcely-Del Carmen, Sofia D.
Vivanco-Hilario, Wilter C. Morales-Garcia.
Project management:
Salazar A Josselyn-Andrea, Salcedo Victcely-Del Carmen, Sofia D.
Vivanco-Hilario, Wilter C. Morales-Garcia.
Resources: Salazar A
Josselyn-Andrea, Salcedo Victcely-Del Carmen, Sofia D. Vivanco-Hilario, Wilter
C. Morales-Garcia.
Software: Salazar A
Josselyn-Andrea, Salcedo Victcely-Del Carmen, Sofia D. Vivanco-Hilario, Wilter
C. Morales-Garcia.
Supervision:
Salazar A Josselyn-Andrea, Salcedo Victcely-Del Carmen, Sofia D.
Vivanco-Hilario, Wilter C. Morales-Garcia.
Validation:
Salazar A Josselyn-Andrea, Salcedo Victcely-Del Carmen, Sofia D.
Vivanco-Hilario, Wilter C. Morales-Garcia.
Display: Salazar A
Josselyn-Andrea, Salcedo Victcely-Del Carmen, Sofia D. Vivanco-Hilario, Wilter
C. Morales-Garcia.
Editor - original draft:
Salazar A Josselyn-Andrea, Salcedo Victcely-Del Carmen, Sofía D.
Vivanco-Hilario, Wilter C. Morales-García.
Writing - proofreading and editing:
Salazar A Josselyn-Andrea, Salcedo Victcely-Del Carmen, Sofía D.
Vivanco-Hilario, Wilter C. Morales-García.
![]() *
*![]()