doi: 10.62486/agmu202463
ORIGINAL
Clinical diagnosis of chronic mucocutaneous candidiasis in a patient with recurrent staphylococcal infections
Diagnóstico clínico de candidiasis mucocutánea crónica en un paciente con infecciones estafilocóccicas recurrentes
Luis Alexis Peláez Yáñez1 *, Odalys Orraca Castillo1, Jessica O. Solana Rodríguez1, Mayelín García García1, Julio Israel Hernández Pacheco1
1Universidad de Ciencias Médicas de Pinar del Río. Hospital Pediátrico Provincial “Pepe Portilla”, Servicio de Inmunología. Pinar del Río. Cuba.
Citar como: Peláez Yáñez LA, Orraca Castillo O, Solana Rodríguez JO, García García M, Hernández Pacheco JI. Clinical diagnosis of chronic mucocutaneous candidiasis in a patient with recurrent staphylococcal infections. Multidisciplinar (Montevideo). 2024; 2:63. https://doi.org/10.62486/agmu202463
Enviado: 20-11-2023 Revisado: 17-04-2024 Aceptado: 11-09-2024 Publicado: 12-09-2024
Editor: Telmo Raúl
Aveiro-Róbalo ![]()
Autor para la correspondencia: Luis Alexis Peláez Yáñez *
ABSTRACT
Chronic mucocutaneous candidiasis is a primary immunodeficiency characterized by persistent or recurrent candidal infections of the skin, nails, or mucous membranes. It can be associated with endocrinopathies and autoimmune diseases. A 37-years-old male patient is presented who attended an immunology consultation referred from the dermatology service due to recurrent pyodermitis of several years of evolution; the physical examination also revealed signs of candidiasis in the oral mucosa and lip corners, in the eyelids of both eyes and skin in the abdominal region, which were recurrent, as well as onychomycosis in all toenails. The microbiological study of the pyodermitis lesions showed infection by staphylococcus aureus, and the lesions of the mouth, eyes, abdominal skin and nails showed the presence of Candida albicans. Delayed intradermal skin testing was performed with no T cell response to Candida and Trichophyton antigens. Complementary drugs were indicated to rule out any associated endocrine disorder.
Keywords: Chronic Mucocutaneous Candidiasis; Primary Immunodeficiency; Recurrent Pyodermitis.
RESUMEN
La candidiasis mucocutánea crónica (CMC) es una inmunodeficiencia primaria que se caracteriza por infecciones candidiásicas persistentes o recurrentes en piel, uñas o membranas mucosas. Puede asociarse con endocrinopatías y con enfermedades autoinmunitarias. Se presenta un paciente masculino de 37 años de edad que asistió a consulta de inmunología remitido desde el servicio de dermatología por presentar piodermitis recurrentes de varios años de evolución; al examen físico se le constató, además, signos de candidiasis en mucosa oral y comisuras labiales, en párpados de ambos ojos y piel de región abdominal, recidivantes, así como onicomicosis en todas las uñas de los pies. El estudio microbiológico de las lesiones por piodermitis arrojó infección por estafilococo dorado, y el de las lesiones de la boca, ojo y piel abdominal y uñas mostraron la presencia de Candida albicans. Se realizaron pruebas cutáneas demoradas intradérmicas sin respuesta de células T a los antígenos de Cándidas y Trichophyton. Se indicaron complementarios para descartar algún trastorno endocrino asociado.
Palabras clave: Candidiasis Mucocutánea Crónica; Inmunodeficiencia Primaria; Piodermitis Recidivante.
INTRODUCTION
CMC comprises a group of diseases with significant clinical heterogeneity characterized by recurrent Candida albicans infections of the skin, nails, and mucous membranes;(1-3) it is classified within the inborn errors of immunity.(4,5)
The disease frequently appears in childhood, although it can occur in adulthood. Patients rarely develop systemic Candida infections, but are more susceptible than immunocompetent individuals to infections by encapsulated bacteria, and the presence of respiratory diseases. Severe complications develop rarely, but infections by Histoplasma capsulatum, Cryptococcus neoformans, or Nocardia have been described. It can be associated with endocrinopathies and autoimmune diseases. Diseases.(2,4,5)
Most cases are sporadic, but there are numerous familial reports. Autosomal dominant and recessive inheritance patterns have been observed.(4)
Cell-mediated immunity is essential in the immune response against Candida sp Recent research detected several immunological defects in IL-17 and its receptors, mutations in signal transducer and activator of transcription factor (STAT 1), and defects already demonstrated in the IL-12-interferon gamma axis.(6,12)
CASE PRESENTATION
Male patient, 37 years old, white, with a personal pathological history of repeated infectious processes; with a history of frequent staphylococcal infections due to forunculosis and recurrent abscesses, with the need for antibiotic therapy, ineffective due to recurrences, for which he was referred to our immunology service.
When we took his medical history, we found that since he was very young, he suffered from respiratory infections such as catarrhal and suppurative otitis media, and also from candidiasis infections of the oral mucosa and skin. Already after one year of age, he began to present skin infections of staphylococcal etiology; on several occasions, he presented diarrhea since childhood. She had synovitis of the knee on many occasions. At the time of the first consultation with our service, the patient had lesions in both labial commissures and abdominal skin, and onychomycosis in all the nails of both feet. It should also be noted that there are vulgar wart lesions on both hands.
This patient required treatment in intensive care wards; at 19 years of age, he was admitted to the intensive care unit of the "Pedro Kourí" Tropical Medicine Institute for cryptococcosis for which he was treated and where it was also necessary to perform a splenectomy "because he had very low hemoglobin and platelet counts" (referred by the patient); at the age of 27, in the intensive care unit of the "Abel Santamaría" Clinical Surgical Hospital of Pinar del Río due to bacterial pneumonia with nosocomial infection of soft parts caused by Pseudomona aeruginosa, where he was treated with several antibiotics such as vancomycin, meropenem and piperacillin with tazobactam.
She came to our office with skin lesions due to the presence of a boil in the anterior medial internal region of the right thigh and with large erythematous, slightly scaly lesions located in the middle and lower ventral abdominal region with continuity to the back and inguinal and gluteal regions, more striking at the level of the folds, associated with intense pruritus (figure 1). The nails of all the toes are thickened and dystrophic (figure 1).
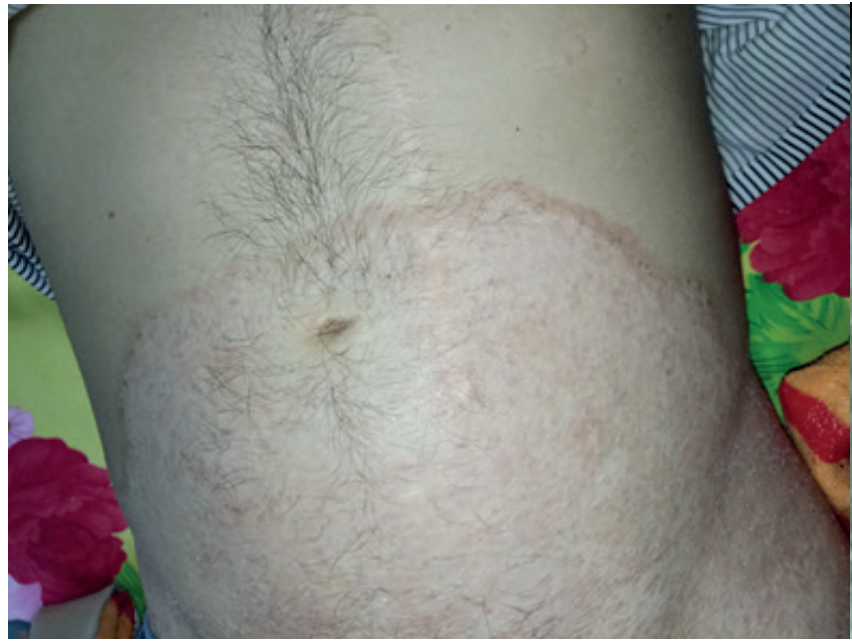

Figure 1. Large erythematous, slightly scaly lesions located in the mid and lower ventral abdominal region with continuity to the back and inguinal and gluteal regions. The nails of all toes are thickened and dystrophic.
Since then, our immunology office has kept this patient under a strict follow-up regimen, during which different studies were performed and the respective therapeutic behavior was indicated.
A microbiological exudate of the furuncle was performed with culture and antibiogram, as well as scraping of the affected skin and nails with culture and antifungal susceptibility test; these complementary tests showed the presence of S. aureus with sensitivity to cotrimoxazole and Candida albicans with positive sensitivity to all antimycotics tested, respectively.
A delayed skin test and an intradermal reaction to Candida and Trichophyton were performed: they were negative at 24, 48; and 72 hours, which indicated a defect in the cellular response mediated by T lymphocytes to Candida sp, mainly.
Other complementary studies performed: leukograms with differential with normal values of leukocytes with amounts of the different white cells within the limits of normality; peripheral lamina, normal; studies of thyroid hormones T3 and T4 as well as TSH yielded normal values; Hepatitis B surface antigen and anti-C antibody tests were negative; HIV ELISA test was negative; C-reactive protein, circulating immunocomplexes and rheumatoid factor tests were negative; HIV ELISA test was negative; and serum immunoglobulin and complement doses were normal: IgG: 15,09g/L(6,80-14,45), IgA: 1,94 g/L(0,83-4,06), IgM: 1,26 g/L(0,34-2,14), IgE 62 IU/L (≤150), C3: 1,12 g/L(0,75-1,35), C4: 0,16 g/L(0,09-0,36)
The hepatic study showed normal TGP and TGO values with figures lower than 25 units per milliliter; the ultrasound showed normal hepatic ultrasonographic values.
Combined oral treatment with cotrimoxazole and rifampicin was started, and Neobatin ointment was applied in the nasal cavities and cohabitants, achieving complete clinical response of furunculosis ten days after starting antibacterial treatment.
After the antibacterial treatment, local and systemic antifungal treatment was started with fluconazole (150 mg) 1 cap daily for 10 days, with clinical improvement. The same dose was then continued weekly for a total of six months, achieving almost total improvement of the skin and nail lesions.
It should be noted that immunostimulation with transfer factor, zinc sulfate, and vitamin therapy was indicated from the beginning of the patient's treatment.
DISCUSSION
We present a patient with CMC with no response to intradermal inoculation of fungal antigens and other associated diseases. The clinical presentation of CMC is very varied, given the heterogeneity of this primary immunodeficiency.(2,4) This suggests that several specific diseases are grouped under the clinical denominator described above.(5)
Between 60 and 80 % of patients with CMC manifest their disease in childhood; only a minority express it late.(3,7,13) Autosomal recessive inheritance predominates, and autosomal dominant inheritance is less frequent. In a minority of cases it presents sporadically; it can be accompanied by endocrinopathies such as hypothyroidism, hypoparathyroidism, Addison's disease, diabetes mellitus and autoimmune processes such as vitiligo, sarcoidosis, pernicious anemia and autoimmune hemolytic anemia,(4,7,14) and it has also been associated with thymoma in adult patients.(7)
Autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy syndrome or APECED, also known as autoimmune polyglandular autoimmune syndrome type 1(15) is transmitted with an autosomal recessive inheritance pattern and is the product of mutations in the autoimmune regulatory gene (AIRE).(7,16) It is characterized by the association of at least two of the following diseases: CMC, hypothyroidism and Addison's disease.(16) Other less frequent manifestations of APECED are autoimmune thyroiditis, gonadal failure, pernicious anemia, type 1 diabetes mellitus, autoimmune hepatitis, chronic diarrhea, malabsorption, and manifestations of ectodermal dystrophy: keratitis, alopecia, dental enamel hypoplasia, and nail dystrophy.(5) Clinical manifestations were not present in this patient until his follow-up.
Within the 10 groups of the classification of inborn errors of immunity,(17) this case most likely corresponds to group VI (defects of innate and intrinsic immunity), given the repeated infectious manifestations with susceptibility to fungal, staphylococcal, and pseudomonas infections presented. Fungal infections characterize group IV diseases (immune dysregulation diseases), but the patient does not show manifestations of dysregulation, such as polyendocrinopathies, typical of these entities, are ruled out.(17)
Among the group VI diseases, those with autosomal recessive inheritance are ruled out since the patient's parents do not have the same surnames and come from different and distant geographical areas, so consanguinity is ruled out; with the possibility of an autosomal dominant inheritance pattern.(17) a new mutation of the gene is present in this case, similar cases are not observed in the ancestry of his family nor the family of his wife, and turn, he has two daughters, one of them healthy and the other sick, being able to corroborate the suspected genetic etiology.
Among the autosomal dominant diseases of group VI (defects in innate and intrinsic immunity), due to the clinical manifestations described, an IL-17F deficiency is suspected, six of which present with an autosomal dominant pattern(10) and are characterized by folliculitis and chronic mucocutaneous candidiasis, eight of which correspond to the patient's clinical picture.(17)
IL-17 is a proinflammatory cytokine secreted mainly by activated T cells. It presents several isoforms (A-F).(3,18) IL-17a is a cytokine characteristic of Th17 cells, although it can be produced by other cell lines such as ϒծ, NKT, and TCD8+ T cells. This cytokine promotes differentiation to the TH17 pattern in defense against extracellular bacteria and fungi and neutrophil migration. Among the IL-17 family members, IL-17F has the highest homology with IL-17A (60 %).(3) The genes coding for IL-17A and IL-17F homodimers of the cytokine IL-17 are clustered on chromosome 14A in mouse and 6pR in human.(6) IL-17A and IL-17F can be secreted as homodimers and heterodimers,(8) with the IL-17A/F heterodimer being more potent than IL-17A in inducing chemokine expression. This cytokine stimulates various cells to produce inflammatory mediators IL-1, TNFα, and other cytokines, necessary for the recruitment of neutrophils and other leukocytes, a characteristic event of inflammation disease.(6,8)
Loss of STAT1 function is another autosomal dominant disease within this group that could be present in the patient under discussion.(9,10,11,12) It is characterized by susceptibility to infections by fungi, bacteria, and viruses, autoimmunity, enteropathies, and endocrine manifestations such as diabetes mellitus and thyroiditis(8,19,20) that are not present in the patient at this time, so it is ruled out.
The management of patients with chronic mucocutaneous candidiasis is based on treating infectious diseases secondary to immune deficiency and associated endocrinopathies and complications.(2) One of the coadjuvant options for the treatment of chronic mucocutaneous candidiasis is transfer factor or dialyzable leukocyte extract, two since clinical improvement of patients with this condition was reported during treatment with transfer factor, seven which was applied with good response in this case and where so far the patient has not presented new infectious complications after our follow-up and treatment.
CONCLUSIONS
Monogenic disorders are now more recognized as associated with increased susceptibility to fungal infections. The findings so far indicate where the knowledge about inborn errors of immunity lies and guide on the path of analysis of immune disorders due to primary immunodeficiencies.
REFERENCES
1. García P, Aquino L, Vega DC, Ortega F, Arenas R. Candidiasis mucocutánea crónica en un paciente con síndrome poliendrocrino autoinmunitario tipo 1. Med Interna Mex. 2022;38(6):1274,1278.
2. Santa Elena AM, Pantoja A, Cisneros N, Addine B de la C, Parada ME. Diagnóstico y evolución de un caso de candidiasis mucocutánea crónica. Available from: http://www.cibamanz2020.sld.cu/index.php/cibamanz/cibamanz2020/paper/view/114/81
3. Venturi P, González A, Carolina AM, Marín C, Angiolini SC, Sotomayor CE. Estudio del perfil Th17 en pacientes pediátricos con candidiasis mucocutánea crónica de la provincia de Mendoza. Arch Alerg e Inmunol Clínica [Internet]. 2022;53:145,156. Available from: https://www.researchgate.net/profile/Claudia-Sotomayor-5/publication/378139417_Th17_profile_in_chronic_mucocutaneous_candidiasis_pediatric_patients_in_Mendoza_province/links/65c8e6cb1e1ec12eff81acac/Th17-profile-in-chronic-mucocutaneous-candidiasis-pediat
4. Ramírez BG, Sáez de Ocaris M del M. Aspectos diagnósticos, fisipatológicos y clínicos de la candidiasis mucocutánea crónica. Revisión de la literatura [Internet]. 2011. Available from: http://repositorio.pediatria.gob.mx:8180/hadle/20.500.12103/1175
5. Egri N, Esteve-Solé A. Deyà-Martínez À, Ortiz de Landazuri I, Vlagea A, García AP. Primary immunodeficiency and chronic mucocutaneous candidiasis: pathophysiological, diagnostic, and therapeutic approaches. Rev Allergol Immunopathol (Madr). 2021;49(1):118-27.
6. Chimenez R, Tropeano A, Chirico V, Ceravolo G, Salpietro C, Cuppari C. IL-17 serum level in patients with chronic mucocutaneous candidiasis disease. Rev Pediatr Allergy Immunol. 2022;33(27):77-9.
7. Chávez MC, Marcelo JL, Gómez Y, González A, Pérez T. Candidiasis mucocutánea crónica. A propósito de un caso. Revista cubana de hematología, inmunología y hemoterapia. 2017;36(suplemento):1-6.
8. Flores C, Bonifaz A. Aspectos inmunológicos de la candidosis mucocutánea crónica. Dermatología Cosmética, Médica y Quirúrgica [Internet]. 2020;18(4):296–305. Available from: https://www.medigraphic.com/pdfs/cosmetica/dcm-2020/dcm204l.pdf
9. Blanco Lobo P, Lei WT, Pelham SJ, Guisado Hernández P, Villaoslada I, de Felipe B. Biallelic TRAF3IP2 variants causing chronic mucocutaneous candidiasis in a child harboring a STAT1 variant. Rev Pediatr Allergy Immunol. 2021;32(8):1804-12.
10. Ostadi V, Sherkat R, Migaud M, Modaressadeghi SM, Casanova JL, Puel A. Functional analysis of two STAT1 gain-of-function mutations in two Iranian families with autosomal dominant chronic mucocutaneous candidiasis. Rev Med Mycol. 2021;59(2):180-8.
11. Carey B, Lambourne J, Porter S, Hodgson T. Chronic mucocutaneous candidiasis due to gain-of-function mutation in STAT1. Rev Oral Dis. 2019;25(3):684-92.
12. Baghad B, Benhsaien I, El Fatoiki FZ, Migaud M, Puel A, Chiheb S. [Chronic mucocutaneous candidiasis with STAT1 gain-of-function mutation associated with herpes virus and mycobacterial infections]. / Candidosecutanéo-muqueusechronique avec mutation gain-de-fonction du gène STAT1 associée à des infections herpétiqueset à mycobactérie. Ann Dermatol Venereol. 2020;147(1):41-5.
13. Frías MG, Rodríguez AC, Torres OU, Acosta G, Martínez E. Epidemiological data of candidiasis in a tertiary hospital in the State of Mexico. Dermatol Rev Mex. 2020;64(2):109-14.
14. García M, Pérez HF, Rojas CM, León X, Llausás E, García C. Chronic mucocutaneous candidiasis associated with autoimmunity and ectodermal dysplasia. A case report. Rev Alerg Mex. 2021;68(2):144-9.
15. Fierabracci A, Arena A, Toto F, Gallo N, Puel A, Migaud M. Autoimmune polyendocrine syndrome type 1 (APECED) in the Indian population: case report and review of a series of 45 patients. Rev J Endocrinol Invest. 2021;44(4):661-77.
16. Candelo PA, Arias DA, Victoria J. Candidiasis mucocutánea generalizada en una paciente con sindrome poliglandular tipo 1. A propósito de un caso. Rev Argentina Dermatología [Internet]. 2019;100. Available from: http://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S1851-300X2019000300101
17. Tangye SG, Al W, Aziz H, Charlotte B, Rundles C, Luis J. Human Inborn Errors of Immunity : 2022 Update on the Classification from the International Union of Immunological Societies Expert Committee Internet. Journal of Clinical Immunology. Springer US; 2022. 1473-1507 p. Available from: https://doi.org/10.1007/s10875-022-01289-3.
18. Verda S, Mirza D, Mallory L, MD Z, Steven R. Inmunidad al error innato de la vía inmunitaria Th17 asociada con la candidiasis mucocutánea crónica: una revisión sistemática. Rev Medicam en dermatología. 2023;22:1197–203.
19. Jobim M, Puel A, Ewald G, Gil BC, Migaud M, Fagundes IS, et al. Nova mutação no gene STAT1 associada com candidíase mucocutânea crônica. Arq Asmas Alerg e Imunol. 2020;4(3):354–9.
20. Chebli de Abreu, Nathalia Duarte S, Hyllo MJ, Neto A. Caso para el diagnóstico. Placas eritematosas y descamativas diseminadas: candidiasis mucocutánea crónica. Sci Direct [Internet]. 2023;98:691–4. Available from: https://www.sciencedirect.com/science/article/pii/S0365059623001101?via%3Dihub
FINANCING
The authors did not receive funding for the development of this research.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Luis Alexis Peláez Yáñez, Odalys Orraca Castillo, Jessica O. Solana Rodríguez, Mayelín García García, Julio Israel Hernández Pacheco.
Data curation: Luis Alexis Peláez Yáñez, Odalys Orraca Castillo, Jessica O. Solana Rodríguez, Mayelín García García, Julio Israel Hernández Pacheco.
Formal analisis: Luis Alexis Peláez Yáñez, Odalys Orraca Castillo, Jessica O. Solana Rodríguez, Mayelín García García, Julio Israel Hernández Pacheco.
Research: Luis Alexis Peláez Yáñez, Odalys Orraca Castillo, Jessica O. Solana Rodríguez, Mayelín García García, Julio Israel Hernández Pacheco.
Methodology: Luis Alexis Peláez Yáñez, Odalys Orraca Castillo, Jessica O. Solana Rodríguez, Mayelín García García, Julio Israel Hernández Pacheco.
Project administration: Luis Alexis Peláez Yáñez, Odalys Orraca Castillo, Jessica O. Solana Rodríguez, Mayelín García García, Julio Israel Hernández Pacheco.
Resourses: Luis Alexis Peláez Yáñez, Odalys Orraca Castillo, Jessica O. Solana Rodríguez, Mayelín García García, Julio Israel Hernández Pacheco.
Software: Luis Alexis Peláez Yáñez, Odalys Orraca Castillo, Jessica O. Solana Rodríguez, Mayelín García García, Julio Israel Hernández Pacheco.
Supervision: Luis Alexis Peláez Yáñez, Odalys Orraca Castillo, Jessica O. Solana Rodríguez, Mayelín García García, Julio Israel Hernández Pacheco.
Validation: Luis Alexis Peláez Yáñez, Odalys Orraca Castillo, Jessica O. Solana Rodríguez, Mayelín García García, Julio Israel Hernández Pacheco.
Visualization: Luis Alexis Peláez Yáñez, Odalys Orraca Castillo, Jessica O. Solana Rodríguez, Mayelín García García, Julio Israel Hernández Pacheco.
Writing –original draft: Luis Alexis Peláez Yáñez, Odalys Orraca Castillo, Jessica O. Solana Rodríguez, Mayelín García García, Julio Israel Hernández Pacheco.
Writing - proofreading and editing: Luis Alexis Peláez Yáñez, Odalys Orraca Castillo, Jessica O. Solana Rodríguez, Mayelín García García, Julio Israel Hernández Pacheco.