doi: 10.62486/agmu202487
ORIGINAL
Psychiatric disorders in patients with epilepsy in the Japanese Hospital and the Dr. Mario Ortíz Suárez Children’s Hospital of Santa Cruz, Bolivia
Trastornos psiquiátricos en pacientes con epilepsia en el Hospital Japonés y el Hospital de Niños Dr. Mario Ortíz Suárez de Santa Cruz, Bolivia
Carmen Julia Salvatierra-Rocha1 ![]() *, Jhossmar Cristians Auza-Santivañez2
*, Jhossmar Cristians Auza-Santivañez2 ![]() *, Giovanna Flores Yucra3
*, Giovanna Flores Yucra3 ![]() *, Carla Patricia Bastos-Vargas4
*, Carla Patricia Bastos-Vargas4 ![]() *, Daniel Ramiro Elías Vallejos-Rejas5
*, Daniel Ramiro Elías Vallejos-Rejas5 ![]() *, Isaura Santander Oberson6
*, Isaura Santander Oberson6 ![]() , Rebeca Rocio Gomez Rosales7
, Rebeca Rocio Gomez Rosales7 ![]()
1Seguro Social Universitario. Santa Cruz, Bolivia.
2Ministerio de Salud y Deportes. Instituto Académico Científico Quispe-Cornejo. La Paz, Bolivia.
3Hospital de Niños “Mario Ortiz Suarez”. Santa Cruz, Bolivia.
4Hospital Japonés. Santa Cruz, Bolivia.
5Facultad de Medicina. Universidad Privada del Valle Bolivia. Santa Cruz, Bolívia.
6Hôspitaé Universitatio de Genève (HUG). Genève, Suiza.
7Hospital infanto juvenil Menino de Jesus M. São Paulo, Brazil.
Cite as: Salvatierra-Rocha CJ, Auza-Santivañez JC, Flores Yucra G, Bastos-Vargas CP, Vallejos-Rejas DRE, Santander Oberson I, et al. Psychiatric disorders in patients with epilepsy in the Japanese Hospital and the Dr. Mario Ortíz Suárez Children’s Hospital of Santa Cruz, Bolivia. Multidisciplinar (Montevideo). 2024; 2:87. https://doi.org/10.62486/agmu202487
Submitted: 07-12-2023 Revised: 02-04-2024 Accepted: 18-08-2024 Published: 19-08-2024
Editor:
Telmo
Raúl Aveiro-Róbalo ![]()
Autor para la correspondencia: Jhossmar Cristians Auza-Santivañez *
ABSTRACT
Introduction: epilepsy is an important neurological disease characterized by stigma, high psychiatric comorbidity, and considerable economic costs. Globally, it is ranked as the second most serious neurological disorder in terms of disability-adjusted life years. In Bolivia, no epidemiological studies have been carried out on psychiatric comorbidity in patients with epilepsy in this context.
Objective: to analyze the sociodemographic variables, identify the most frequent psychiatric disorders and determine the association between these disorders and the type of epilepsy, in patients with epilepsy treated in outpatient clinics in tertiary hospitals in Santa Cruz.
Method: this study is observational, descriptive, analytical, retrospective, cross-sectional and multicenter. The study population included all patients with a diagnosis of epilepsy seen in an outpatient Neurology clinic, with a concurrent diagnosis of psychiatric disorders. A non-probabilistic sample was used to collect data, which was obtained through the review of medical records and statistical records, using a structured data collection form.
Results and discussion: according to the data obtained, an equitable distribution is observed between both sexes. Regarding age, adults predominate followed by children. Regarding education, the majority of participants have primary education, followed by secondary education. The other educational levels (preschool, middle/higher technical, university, and special education) have smaller representations. The relationship between education and age shows that the majority of adults have primary education. Regarding the etiology of epilepsy, the unknown cause predominates, followed by the structural cause and the genetic cause. Regarding the type of epilepsy, the most common is generalized, followed by seal and combined. In psychiatric diagnosis, the most common disorder is mental retardation.
Conclusions: the results highlight the high prevalence of mental retardation in its different degrees and depressive disorder among patients with epilepsy. The etiology of epilepsy, the unknown cause predominates, followed by the structural cause and the genetic cause. In psychiatric diagnosis, the most common disorder is mental retardation. More epidemiological studies are required to further evaluate psychiatric comorbidity in patients with epilepsy, which could inform better clinical management and intervention strategies.
Keywords: Psychiatry; Epilepsy; Depression; Comorbidity; Diagnosis; Mental Health; Psychiatric Disorders in Epilepsy.
RESUMEN
Introducción: la epilepsia es una enfermedad neurológica importante que se caracteriza por el estigma, la alta comorbilidad psiquiátrica y costos económicos considerables. A nivel global, se clasifica como el segundo trastorno neurológico más grave en términos de años de vida ajustados por discapacidad. En Bolivia no se han llevado a cabo estudios epidemiológicos sobre la comorbilidad psiquiátrica en pacientes con epilepsia en este contexto.
Objetivo: analizar las variables sociodemográficas, identificar los trastornos psiquiátricos más frecuentes y determinar la asociación entre estos trastornos y el tipo de epilepsia, en pacientes con epilepsia atendidos en consulta externa en hospitales de tercer nivel en Santa Cruz.
Método: este estudio es observacional, descriptivo, analítico, retrospectivo, transversal y multicéntrico. La población de estudio incluyó a todos los pacientes con diagnóstico de epilepsia atendidos en consulta externa de Neurología, con diagnóstico concurrente de trastornos psiquiátricos. Se utilizó una muestra no probabilística para la recolección de datos, los cuales se obtuvieron a través de la revisión de historias clínicas y registros estadísticos, utilizando una ficha de recolección de datos estructurada.
Resultados y discusión: de acuerdo con los datos obtenidos, se observa una distribución equitativa entre ambos sexos. Respecto a la edad, predominan los adultos seguidos por los niños. En cuanto a la escolaridad, la mayoría de los participantes tienen educación primaria, seguida por secundaria. Los demás niveles educativos (pre-escolar, técnico medio/superior, universitario, y educación especial) tienen representaciones menores. La relación entre escolaridad y edad muestra que la mayoría de los adultos tienen educación primaria. En cuanto a la etiología de la epilepsia, predomina la causa desconocida, seguida de la causa estructural y la causa genética. En cuanto al tipo de epilepsia, la más frecuente es la generalizada, seguida de la foca y la combinada. En el diagnóstico psiquiátrico, el trastorno más común es el retraso mental.
Conclusiones: Los resultados destacan la alta prevalencia de retraso mental en sus diferentes grados y trastorno depresivo entre los pacientes con epilepsia. La etiología de la epilepsia, predomina la causa desconocida, seguida de la causa estructural y la causa genética. En el diagnóstico psiquiátrico, el trastorno más común es el retraso mental. Se requieren más estudios epidemiológicos para profundizar en la evaluación de la comorbilidad psiquiátrica en pacientes con epilepsia, lo que podría informar mejores estrategias de intervención y manejo clínico.
Palabras clave: Psiquiatría; Epilepsia; Depresión; Comorbilidad; Diagnóstico; Salud Mental; Desordenes Psiquiátricos en Epilepsia.
INTRODUCTION
Epilepsy is a serious neurological condition associated with stigma, psychiatric comorbidity, and considerable economic costs. According to a 2010 WHO Global Burden of Disease study, epilepsy is the second most serious neurological disorder globally in terms of disability-adjusted life years. People with epilepsy have a higher incidence of psychiatric disorders compared to the general population and other chronic medical conditions,(1-3) highlighting the importance of early identification and treatment of these disorders to improve seizure control, reduce adverse effects, improve quality of life, as well as reduce healthcare costs and improve social outcomes.
Some studies show an incidence of between 26 and 70 per 100 000 inhabitants, while in developing countries, it is approximately 100 per 1 000. In 37 studies conducted in Latin America and the Caribbean, the rates of active epilepsy, without adjustment for age, varied between 3,4 per 1 000.(4)
In Bolivia, despite the existence of a law protecting people with disabilities and a draft law on mental health under discussion in the Chamber of Deputies since March 2023,(5) no epidemiological studies have been conducted on psychiatric comorbidity with epilepsy. In tertiary hospitals, it is common to see patients diagnosed with epilepsy who have psychiatric disorders in outpatient consultations, but their frequency and association are unknown. This study aims to characterize psychiatric disorders in patients with epilepsy seen in outpatient consultations in tertiary hospitals in Santa Cruz, the Japanese Hospital. The Dr. Mario Ortíz Suárez Children's Hospital analyzes sociodemographic variables, identifies the most frequent psychiatric disorders, and determines the association between these disorders and the type of epilepsy to highlight the seriousness of this problem and improve medical care and outcomes for these patients.(6,7)
METHOD
Study design: Observational, descriptive, analytical, retrospective, and cross-sectional, from January to December 2023.
Research methods and techniques: Review of medical records and statistical records from hospitals. Universe: All patients seen in outpatient clinics with a diagnosis of epilepsy in the neurology department. Inclusion criteria: Patients diagnosed with epilepsy and psychiatric disorders, according to ICD-10. Exclusion criteria: Undefined psychiatric diagnosis. Variables: age, sex, education, etiology of epilepsy, type of epilepsy, psychiatric diagnosis.
Data collection: Data were collected using a form containing variables obtained from medical records, including age, sex, education, etiology, and type of epilepsy, as well as psychiatric diagnosis, for all patients diagnosed with epilepsy who were admitted to the adult and pediatric neurology outpatient clinic and met the inclusion criteria during the study period.
Data analysis. The sociodemographic characteristics of the patients studied were described using the Report package version 0.4.0. Qualitative variables (type of epilepsy and psychiatric diagnosis) were compared using Pearson's chi-square test (χ2); the effect size was determined by calculating Vcramer, categorizing its significance as suggested by Cohen (1988). The existence of statistical significance in all analyses performed was determined based on a rejection alpha of 0,05 (α=0,05). Statistical contrast for qualitative and quantitative variables was performed and graphed using the SPSS statistical package.
RESULTS AND DISCUSSION
According to the data obtained, there is an equal distribution between both sexes, with females representing 50,3 % (n=72) and males 49,7 % (n=71). In terms of age, adults predominate (55,9 %, n=80), followed by children (41,3 %, n=59) and a minority of older adults (2,8 %, n=4), reflecting a significantly lower representation of the latter category. In terms of education, most participants had primary education (49,0 %), followed by secondary education (25,2 %), and 17,5 % were not enrolled in school. Other educational levels (preschool, technical/higher education, university, and special education) had lower representations, all below 4 % (table 1).
|
Table 1. Sociodemographic characteristics |
||
|
Sex |
||
|
Female (n=72) |
|
Male (n=71) |
|
50,3 |
|
49,7 |
|
Age |
|
|
|
Children (n=59) |
Adult (n=80) |
Elderly person (n=4) |
|
41,3 |
55,9 |
2,8 |
|
Schooling |
|
|
|
Preschool |
|
3,5 |
|
Primary |
|
49,0 |
|
Secondary |
|
25,2 |
|
Medium/Senior Technician |
|
1,4 |
|
University student |
|
1,4 |
|
Not in school |
|
17,5 |
|
Special Education |
|
2,1 |
The relationship between education and age shows that most adults have primary education (28,6 %), followed by secondary education (20 %), with a minimal proportion having university education (1,4 %) or higher technical education (0,7 %). The chi-square test revealed a two-tailed significance of 0.000 (<0,05), indicating a statistically significant relationship between education and age (figure 1).
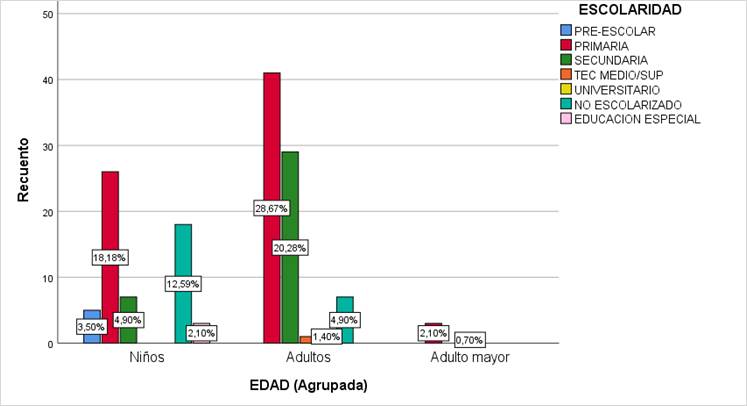
Figure 1. Relationship between age groups and schooling.
Note: Bilateral significance: 0,000 <0.05
The relationship between age and gender does not show a significant trend, as the chi-square test yielded a bilateral significance of 0,116 (>0,05). This indicates that there is no statistically significant association between age and gender in the sample analyzed (figure 2).
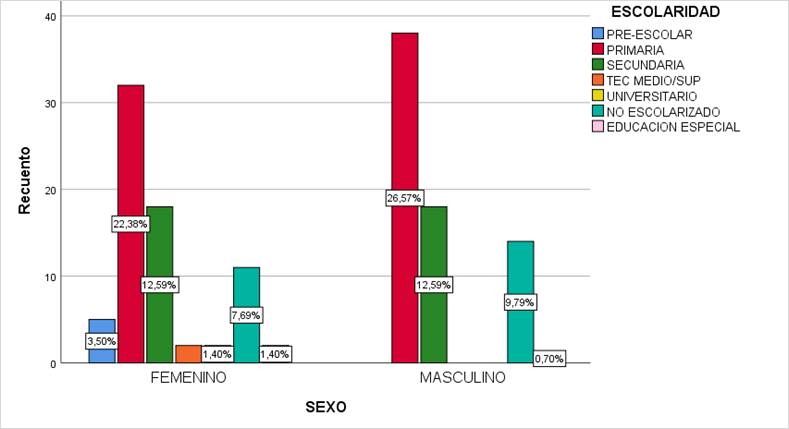
Figure 2. Relationship between age groups and sex.
Note: Bilateral significance: 0,116 >0,05
Regarding the etiology of epilepsy, unknown causes predominate with 49 %, followed by structural causes with 33,5 % and genetic causes with 12,5 % (figure 3). In terms of the type of epilepsy, the most common is generalized epilepsy, accounting for 56,6 %, followed by focal epilepsy, accounting for 18,8 %, and combined epilepsy, accounting for 13,99 % (figure 4).
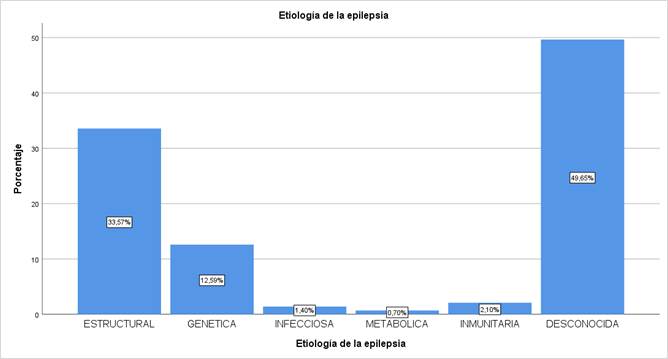
Figure 3. Etiology of epilepsy
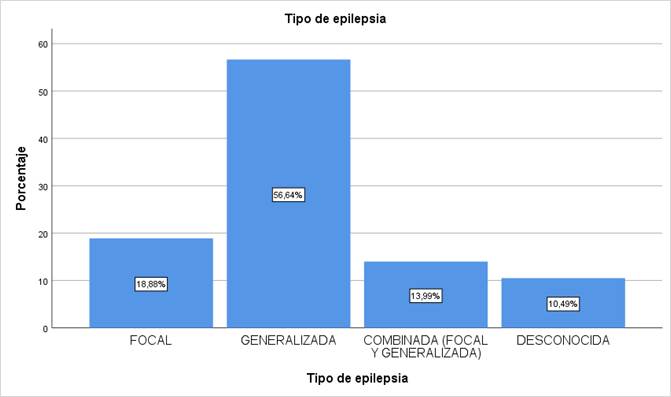
Figure 4. Type of epilepsy
In psychiatric diagnosis, the most common disorder is mental retardation, accounting for 47,6 % of cases. Mental retardation is divided into mild (14,7 %), moderate (21 %), and severe (11,9 %) cases, followed by depressive disorder (9,1 %) and school learning development disorder (7,0 %). Other diagnoses have lower frequencies, including mixed anxiety-depressive disorders (4,9 %), anxiety (6,3 %), psychosis (4,9 %), conduct disorder (5,6 %), ADHD (4,9 %), language disorder (5,6 %), and others (4,2 %) (table 2).
|
Table 2. Type of psychiatric diagnosis |
|||||
|
|
Diagnostico psiquiátrico |
|
Frecuency |
|
Percentage |
|
|
Depressive Disorder |
|
13 |
|
9,1 |
|
Mixed Disorder (Anxious-Depressive) |
|
7 |
|
4,9 |
|
|
Anxiety Disorder |
|
9 |
|
6,3 |
|
|
Psychosis |
|
7 |
|
4,9 |
|
|
School Learning Development Disorder |
|
10 |
|
7,0 |
|
|
Behavioral Disorder |
|
8 |
|
5,6 |
|
|
ADHD |
|
7 |
|
4,9 |
|
|
Language Disorder |
|
8 |
|
5,6 |
|
|
Other |
|
6 |
|
4,2 |
|
|
Mental Retardation |
|
68 |
|
47,6 |
|
|
Mild |
Moderate |
|
Severe |
|
|
|
14,7 |
21 |
|
11,9 |
|
|
|
Total |
|
143 |
|
100,0 |
|
An analysis of the relationship between the type of psychiatric diagnosis and age was conducted, which showed that mental retardation affects 12,6 % of children, 34,3 % of adults, and 0,7 % of older adults. The chi-square value obtained was 0,000; indicating statistical significance (<0,05) and pointing to a statistically significant association between the type of psychiatric diagnosis and age. On the other hand, the relationship between the type of psychiatric diagnosis and gender showed that mental retardation affects 21,7 % of women and 25,9 % of men. The chi-square value obtained was 0,015; which is statistically significant (p < 0,05). This indicates that there is a significant association between the diagnosis of mental retardation and gender in the sample analyzed (table 3).
|
Table 3. Type of psychiatric diagnosis Age – Sex |
|||||||
|
Psychiatric Diagnosis
|
|
Age (Grouped) |
Sex |
Total |
|||
|
Children |
Adults |
Elderly person |
Feminine |
Male |
|||
|
Depressive Disorder |
Recount |
5 |
8 |
0 |
6 |
7 |
13 |
|
% of total |
3,5 % |
5,6 % |
0,0 % |
4,2 % |
4,9 % |
9,1 % |
|
|
Mixed Disorder (Anxiety-Depressive) |
Recount |
0 |
6 |
1 |
7 |
0 |
7 |
|
% of total |
0,0 % |
4,2 % |
0,7 % |
4,9 % |
0,0 % |
4,9 % |
|
|
Mental Retardation |
Recount |
18 |
49 |
1 |
31 |
37 |
68 |
|
% of total |
12,6 % |
34,3 % |
0,7 % |
21,7 % |
25,9 % |
47,6 % |
|
|
Anxiety Disorder |
Recount |
3 |
6 |
0 |
6 |
3 |
9 |
|
% of total |
2,1 % |
4,2 % |
0,0 % |
4,2 % |
2,1 % |
6,3 % |
|
|
Psychosis |
Recount |
0 |
5 |
2 |
2 |
5 |
7 |
|
% of total |
0,0 % |
3,5 % |
1,4 % |
1,4 % |
3,5 % |
4,9 % |
|
|
School Learning Development Disorder
|
Recount |
8 |
2 |
0 |
7 |
3 |
10 |
|
% of total |
5,6 % |
1,4 % |
0,0 % |
4,9 % |
2,1 % |
7,0 % |
|
|
Behavioral Disorder
|
Recount |
7 |
1 |
0 |
7 |
1 |
8 |
|
% of total |
4,9 % |
0,7 % |
0,0 % |
4,9 % |
0,7 % |
5,6 % |
|
|
ADHD
|
Recount |
7 |
0 |
0 |
2 |
5 |
7 |
|
% of total |
4,9 % |
0,0 % |
0,0 % |
1,4 % |
3,5 % |
4,9 % |
|
|
Language Disorder
|
Recount |
6 |
2 |
0 |
3 |
5 |
8 |
|
% of total |
4,2 % |
1,4 % |
0,0 % |
2,1 % |
3,5 % |
5,6 % |
|
|
Others |
Recount |
5 |
1 |
0 |
1 |
5 |
6 |
|
Total
|
% of total |
3,5 % |
0,7 % |
0,0 % |
0,7 % |
3,5 % |
4,2 % |
|
Recount |
59 |
80 |
4 |
72 |
71 |
143 |
|
|
% of total |
41,3 % |
55,9 % |
2,8 % |
50,3 % |
49,7 % |
100,0 % |
|
|
Chi-Cuadrado de Pearson |
Asymptotic significance (bilateral) |
0,000 <0,05 |
0,015 <0,05 |
||||
CONCLUSIONS
The results highlight the high prevalence of mental retardation in its various degrees and depressive disorder among patients with epilepsy, underscoring the need for comprehensive management. About age, adults predominate, followed by children. Most participants have primary education, followed by secondary education. The etiology of epilepsy is predominantly unknown, followed by structural and genetic causes. In psychiatric diagnosis, the most common disorder is mental retardation, followed by school learning development disorder. The close bidirectional relationship between psychiatric disorders and epilepsy, observed in all age groups and sexes, underscores the importance of integrating this knowledge into medical practice and the training of health personnel involved in the care of patients with neurological and mental health conditions.
Further epidemiological studies are needed to further assess psychiatric comorbidity in patients with epilepsy, which could inform better intervention and clinical management strategies.
REFERENCES
1. Gaitatzis A, Trimble MR, Sander JW. The psychiatric comorbidity of epilepsy. Acta Neurol Scand. 2004;110(4):207–20. http://dx.doi.org/10.1111/j.1600-0404.2004.00324.x
2. Doss RC, LaFrance WC Jr. Psychogenic non‐epileptic seizures. Epileptic Disord. 2016 18(4):337–43. https://doi.org/10.1684/epd.2016.0873
3. LaFrance WC jr, Kanner AM, Hermann B. Chapter 20 psychiatric comorbidities in epilepsy. International Review of Neurobiology. Elsevier; 2008. p. 347–83. https://doi.org/10.1016/S0074-7742(08)00020-2
4. Acevedo C, Miranda C, Campos M, Caraballo R, Carpio A, Cuadra L, et al. Informe sobre la epilepsia en Latinoamérica. Washington: OPS; 2008. https://www.paho.org/hq/dmdocuments/2008/Informe_sobre_epilepsia.pdf
5. Cámara de diputados. Proyectos de Ley Legislatura 2023-2024. PL No 310/2023-2024. https://diputados.gob.bo/proyectos-de-ley-en-tratamiento/
6. Mioramalala S, Mroueh L, Bruand P-E, Raharinivo MM, Rafanomezantsoa RM, Gérard D, et al. Effects of an intervention program to improve mental health and epilepsy care in Madagascar. Compr Psychiatry. 2024;132(152484):152484. http://dx.doi.org/10.1016/j.comppsych.2024.152484
7. Kerr MP, Mensah S, Besag F, de Toffol B, Ettinger A, Kanemoto K, et al. International consensus clinical practice statements for the treatment of neuropsychiatric conditions associated with epilepsy: Treatment of Neuropsychiatric Conditions Associated with Epilepsy. Epilepsia. 2011;52(11):2133–8. http://dx.doi.org/10.1111/j.1528-1167.2011.03276.x
FINANCING
The authors did not receive funding for the implementation of this study.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Carmen Julia Salvatierra-Rocha.
Formal analysis: Carmen Julia Salvatierra-Rocha, Jhossmar Cristians Auza-Santivañez.
Research: Jhossmar Cristians Auza-Santivañez.
Methodology: Jhossmar Cristians Auza-Santivañez, Isaura Santander Oberson, and Rebeca Rocio Gomez Rosales.
Project management: Giovanna Flores Yucra.
Supervision: Carmen Julia Salvatierra-Rocha, Daniel Ramiro Elías Vallejos-Rejas.
Visualization: Daniel Ramiro Elías Vallejos-Rejas.
Writing – original draft: Carmen Julia Salvatierra-Rocha, Jhossmar Cristians Auza-Santivañez, Giovanna Flores Yucra, Carla Patricia Bastos-Vargas, Daniel Ramiro Elías Vallejos-Rejas, Isaura Santander Oberson, and Rebeca Rocio Gomez Rosales.
Writing, review, and editing: Carmen Julia Salvatierra-Rocha, Jhossmar Cristians Auza-Santivañez, Giovanna Flores Yucra, Carla Patricia Bastos-Vargas, Daniel Ramiro Elías Vallejos-Rejas, Isaura Santander Oberson, and Rebeca Rocio Gomez Rosales.