doi: 10.62486/agmu202488
CASE REPORT
Giant multiloculated omental cyst in a pediatric patient. Case report and literature review
Quiste gigante de epiplón multiloculado en paciente pediátrico. Reporte de caso y revisión de la bibliografía
Giovanni Callizaya Macedo1
 *,
Jhossmar Cristians Auza-Santivañez2
*,
Jhossmar Cristians Auza-Santivañez2
 *,
Daniel Ramiro Elías Vallejos Rejas3
*,
Daniel Ramiro Elías Vallejos Rejas3
 *,
Ritdber Alfredo Quispe Sarmiento4
*,
Ritdber Alfredo Quispe Sarmiento4
 *,
Jhaleny Jael Flores Canaviri5
*,
Jhaleny Jael Flores Canaviri5
 *,
Liliana Heydi Suarez Laime6
*,
Liliana Heydi Suarez Laime6
 *
*
1 Hospital del Niño “Dr. Ovidio Aliaga Uría”. La Paz. Bolivia.
2 Ministerio de Salud y Deportes. Instituto Académico Científico Quispe-Cornejo. La Paz. Bolivia.
3 Facultad de Medicina. Universidad Privada del Valle Bolivia. Santa Cruz. Bolivia.
4 Hospital Daniel Bracamonte. Potosí. Bolivia.
5 Seguro Social Universitario, Cochabamba. Bolivia.
6 Hospital Materno Infantil German Urquidi. Cochabamba. Bolivia.
Cite as: Callizaya Macedo G, Auza-Santivañez JC, Vallejos Rejas DRE, Quispe Sarmiento RA, Flores Canaviri JJ, Suarez Laime LH. Giant multiloculated omental cyst in a pediatric patient. Case report and literature review. Multidisciplinar (Montevideo). 2024; 2:88. https://doi.org/10.62486/agmu202488
Submitted: 08-12-2023 Revised: 03-04-2024 Accepted: 05-08-2024 Published: 06-08-2024
Editor: Telmo
Raúl Aveiro-Róbalo ![]()
Corresponding author: Jhossmar Cristians Auza-Santivañez *
ABSTRACT
Introduction: omental cysts are rare intra-abdominal lesions, with a frequency of 1:250 000, which often present asymptomatically. However, they can cause abdominal distension, or even surgical abdominal symptoms.
Case report: a 3-year-old female patient presents with a clinical picture of 2 years of evolution, reporting progressive abdominal distention since she was one year old and abdominal pain for 2 weeks. Physical findings show an abdomen with great abdominal distention, tense and painful on superficial and deep palpation. A contrast-enhanced CT scan of the abdomen and pelvis revealed abdominopelvic cystic lesions. Exploratory laparotomy revealed a giant multilocular cystic mass dependent on the greater omentum. The pathological report revealed a giant omentum cyst. A successful surgical resection of the cystic lesions was performed and a favorable post-surgical evolution was performed.
Conclusions: omentum cysts are rare in paediatrics. Diagnosis is based on imaging studies and is confirmed during surgery. Surgical treatment is effective and with few complications.
Keywords: Omental Cyst; Ascites; Abdominal Masses; Mesentery Cyst.
RESUMEN
Introducción: los quistes de epiplón son lesiones intraabdominales raros, con una frecuencia de 1:250 000, que a menudo se presentan de manera asintomática. Sin embargo, pueden causar distensión abdominal, o incluso un cuadro abdominal quirúrgico.
Caso clínico: paciente femenina de 3 años de edad, presenta un cuadro clínico de 2 años de evolución, refiriendo distención abdominal de manera progresiva desde el año de edad y dolor abdominal desde hace 2 semanas. En hallazgos físicos, presenta abdomen con gran distensión abdominal, tenso y doloroso a la palpación superficial y profunda. Se realiza TAC de abdomen y pelvis con contraste que informa lesiones quísticas abdominopélvicas. A laparotomía exploratoria se evidencia masa quística gigante multilocular dependiente del epiplón mayor. Al informe anatomopatológico se reporta un quiste gigante de epiplón. Se realizó una resección quirúrgica exitosa de las lesiones quísticas y evolución postquirúrgica favorable.
Conclusiones: los quistes de epiplón son raros en pediatría. El diagnóstico se basa en estudios de imagen y se confirma durante la cirugía. El tratamiento quirúrgico es efectivo y con pocas complicaciones
Palabras clave: Quiste De Epiplón; Ascitis; Masas Abdominales; Quiste Del Mesenterio.
INTRODUCTION
According to the literature, omentum cysts (OC) are rare intra-abdominal formations with an estimated incidence of approximately 1:200 000 to 1:250 000 in pediatric admissions.(1,2,3) These cysts were first described by Gairdner in 1852. They are caused by a benign proliferation of ectopic lymphatic vessels that lack communication with the lymphatic system, which can manifest clinically as large-volume ascites, thus complicating diagnosis.(4,5)
These cysts are significantly less common than mesenteric cysts, up to ten times more frequent, with an incidence of 1:20 000.(1,6) Diagnosis can be challenging given their rarity and nonspecific clinical presentation. Imaging techniques such as ultrasound and computed axial tomography (CAT) with intravenous contrast are useful for identifying these lesions, with definitive diagnosis confirmed intraoperatively. Other imaging techniques, such as magnetic resonance imaging, are also available. Their more significant advantage in pediatrics is highlighted as they do not involve ionizing radiation, but their high cost limits their routine use.
We present the case of a 3-year-old pediatric patient with a giant multilocular omental cyst—the patient presented with progressive abdominal distension and moderate abdominal pain that had been present for 2 weeks. The diagnosis was confirmed by exploratory laparotomy, and successful surgical resection of the cystic lesions was performed, with favorable postoperative evolution.
CLINICAL CASE
A 3-year-old female patient, resident in the rural area of Los Yungas – La Paz, Bolivia, was transferred from primary care with a clinical history of approximately 2 years, characterized by progressive abdominal distension since she was 1 year old for the past 2 weeks, she has been experiencing moderate abdominal pain. On physical examination upon admission, the positive findings include a greatly distended abdomen, tense and painful on superficial and deep palpation, no peritoneal irritation, abdominal circumference of 75 cm, positive ascites, and hypoactive bowel sounds.
Upon admission, the patient’s laboratory results were as follows: hematocrit (Hct) 37 %, hemoglobin (Hb) 12,2 g/dL, GB: 11,900 mm3, segmented: 78 %, platelets: 759,000 mm3, total bilirubin: 0,5 mg/dL BD: 0,2 mg/dL BI: 0,2 mg/dL. Glutamic oxaloacetic transaminase (GOT): 28,6 mg/dL. Glutamic pyruvic transaminase (GPT): 8,9 IU/L, alkaline phosphatase (ALP): 196 IU/L, blood glucose: 74,2 mg/dL, creatinine: 0,4 mg/dL, urea: 20,3 mg/dL, NUS: 9,4 mg/dL, uric acid: 3,5 mg/dL, calcium: 7,4 mg/dL, total protein: 8,7 mg/dL, albumin: 3,3 mg/dL, magnesium: 1,4 mg/dL, phosphorus: 4,2 mg/dL, Gamma-Glutamyltransferase (GGT): 12,6 mg/dL, Cholesterol: 125,5 mg/dL, Triglycerides: 110,3 mg/dL, Polymerase Chain Reaction (PCR): 19,2 mg/dL, TP: 11 seconds, activity: 100 %, General Urine Test: no abnormalities, coproparasitological: Presence of Giardia Lamblia trophozoites, Entamoeba coli cysts, which was treated with Metronidazole at 41 mg/kg/day for 7 days.
An abdominal ultrasound was performed, which reported significant free intra-abdominal fluid (ascites) displacing abdominal organs into the thoracic cavity, with no evidence of alterations in the organs themselves.
For a comprehensive approach to the patient, multidisciplinary management was carried out with the Pediatrics, Gastroenterology, Infectious Diseases, Oncology, and Pediatric Surgery departments. Hepatic etiology was ruled out as the cause of ascites, as the liver profile was not altered. The approach was completed with tumor markers AFP: 6,9 IU/mL and BHCG: 0,3 mIU/mL, which were negative for suspected neoplasia. Gen-Xpert was reported as negative, so tuberculosis was also ruled out in this patient.
An abdominal and pelvic CT scan with intravenous contrast was performed, which reported the formation of multiple confluent abdominopelvic cystic lesions on the right side measuring 16,2 x 10 x 20 cm (T x AP x L) with an approximate volume of 648 cc and on the left side with a lobulated appearance measuring 10,5 x 10,4 x 21 cm. (T x AP x L) with an approximate volume of 1005 cc, showing thin internal septa that enhance slightly in the arterial phase. The third cystic lesion extends into the left subphrenic space, measuring 10,8 x 5,5 x 11,2 cm. (T x AP x L) with an approximate volume of 370 cc. Multilocular lesions exert a significant mass effect on the head and towards the periphery of the adjacent structures. (figure 1)
Findings are suggestive of septated cystic ovarian lesions, probable bilateral serous/mucinous cystadenoma, and hydatid cysts. For this reason, surgical admission to our pediatric surgery unit was scheduled for exploratory laparotomy and management, according to the findings.
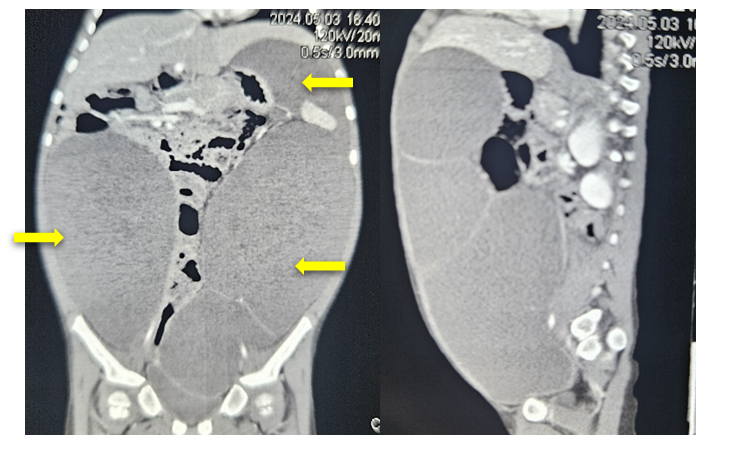
Figure 1. Abdominal and pelvic CT scan with intravenous contrast, showing homogeneous hypodense images with fluid density compatible with abdominal-pelvic cystic lesions (arrows) on the right side measuring 16,2 x 10 x 20 cm. On the left side, a multilocular lesion measuring 10,5 x 10,4 x 21 cm is observed, and the third cystic lesion extends into the left subphrenic space, measuring 10,8 x 5,5 x 11,2 cm.
Surgical treatment:
A midline supra- and infra-umbilical incision is made, followed by dissection in layers down to the cavity, revealing a giant multilobulated cystic mass dependent on the greater omentum, occupying a large part of the abdominal cavity and displacing neighboring structures. The cystic lesions are resected along with a large part of the greater omentum, which has a volume of approximately 4200 ml. The adnexa is examined and found to be unaltered. An incidental appendectomy is also performed. The procedures are uneventful. (figure 2A – 2B)
The pathological anatomy report indicates a giant omentum cyst measuring 18,5 x 12,0 x 4,0 cm, with cholesterol crystal deposits and a foreign body inflammatory reaction, chronic subacute inflammation of the omentum, with no criteria for malignancy.
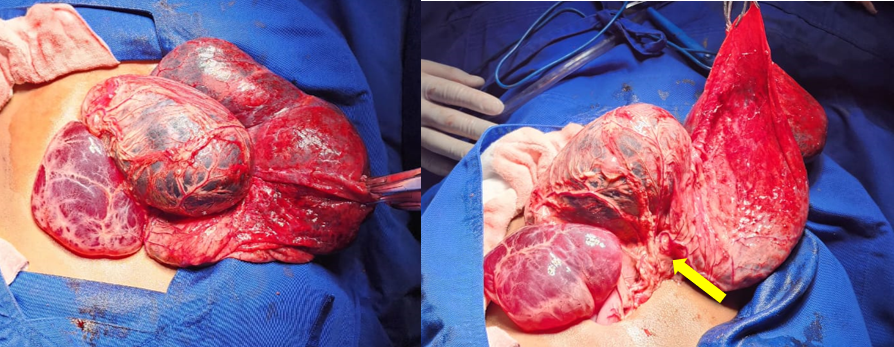
Figure 2. A. Intraoperative image showing giant cystic lesions. B. Image showing that the cysts are completely dependent on the greater omentum (arrows).
She’s doing well after surgery, so she was discharged on the 5th day after surgery for follow-up at the pediatric surgery outpatient clinic.
DISCUSSION
Omentum cysts are rare intra-abdominal lesions and can develop as an asymptomatic mass because they do not cause any symptoms. The clinical picture presents as an asymptomatic palpable abdominal mass. It may be accompanied by nonspecific symptoms such as abdominal distension and pain, although in some cases, it may initially present as a surgical abdominal condition.
The incidence of omentum cysts varies between 1:200 000 and 250 000 pediatric hospital admissions, with mesenteric cysts being much more common. They occur more frequently in females and preschoolers, as with our patients. (1,2,3,6)
The diagnosis is made based on the clinical picture and imaging studies. Although abdominal ultrasound is the test of choice, the diagnosis is often difficult, with nonspecific findings such as ascites on ultrasound, especially when the presentation is unilocular or very thin septa, as in our reported case.(7) CT should be able to define the organ of origin of the cyst. Still, in our patient, it was not accurate, reporting another origin of the lesion due to its large volume, which shows that the diagnosis was established intraoperatively when the greater omentum was identified as the origin of the cystic lesions. It is important to note that during the initial phase of formation, diagnosis by routine transabdominal ultrasound usually concludes with intra-abdominal incidentalomas.
It is interesting to highlight the late diagnosis in our case since although the mother noticed abdominal distension from the age of one, she did not give it the necessary importance to seek medical attention. This is common in rural areas of our country, in this case, the Yungas region of La Paz, where it is common to resort to home remedies and traditional medicine as first-line treatments. For this reason, the patient presented with symptoms that had been evolving for two years before her definitive diagnosis.
The differential diagnosis should include intra-abdominal cystic masses such as ovarian cysts, hydatid cysts, mesenteric cysts,
Surgical resection of the cyst is the treatment of choice in these cases and was the approach taken in our case. Recurrences and/or complications are rare.
CONCLUSIONS
Multilocular giant omentum cysts are rare in children. Diagnosis is established based on clinical presentation and imaging studies, with a definitive diagnosis confirmed during surgery upon confirmation of the origin of the cysts. The results of surgical treatment for this type of pathology are very favorable, with few complications and low recurrence rates.
REFERENCES
1. Al Varado García DRR, Vargas DREU, Aliñas DRSF, Gallego Grijalva DRJ. Quistes de epiplón y mesenterio en niños [Internet]. Gob.mx:8180. 2001. Disponible en: http://repositorio.pediatria.gob.mx:8180/bitstream/20.500.12103/1367/1/ActPed2001_46.pdf
2. Fernández Ramos J, Vázquez Rueda F, Azpilicueta Idarreta M, Díaz Aguilar C. Quiste mesotelial gigante de omento mayor. An Pediatr (Barc) [Internet]. 2009;71(2):180–1. Disponible en: https://doi.org/10.1016/j.anpedi.2009.05.003
3. La Parra Márquez M, Prado I, Gaona D, Arzoz Gálvez M, Lopez Martínez R. Quiste gigante de epiplón: informe de un caso en un sujeto pre-escolar. Cirujano General 2004. Disponible en: https://www.medigraphic.com/pdfs/imss/im-2010/im105p.pdf
4. Nett MH, Vo NJ, Chapman T. Large omental cyst. Radiol Case Rep [Internet]. Available at: https://doi.org/10.2484/rcr.v5i2.388
5. Zurita DÁ, Peñarreta y E. Zambrano L. Quiste gigante de epiplón en niños [Internet]. Org.ar. [citado el 24 de junio de 2024]. Disponible en: https://acacip.org.ar/revista-cirugia-infantil/indice-29/docs/12-Quiste-gigante-de-epiplon-en-ninos.pdf
6. Álvarez-Solís RM, Francisco-Javier Chagolla-Santillán, Quero-Hernández A, et al. Quistes de mesenterio y epiplón en niños. Estudio clínico de 21 casos. Pediatr Mex. 2009;11(1):20-23. Disponible en: https://www.medigraphic.com/pdfs/conapeme/pm-2009/pm091g.pdf
7. Robbins KJ, Antiel RM, Shakhsheer BA. Omental cyst: a case report and review of the literature. Ann Pediatr Surg [Internet]. Available at: https://doi.org/10.1186/s43159-021-00129-0
CONSENT
The patient’s consent was obtained for the performance of this work.
FINANCING
The authors did not receive funding for the implementation of this study.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.