doi: 10.62486/agmu202489
ORIGINAL
Nursing process for a patient with ectopic pregnancy in the Gynecology Department of a hospital in Arequipa
Proceso de enfermería a paciente con embarazo ectópico del Servicio de Ginecología de un hospital de Arequipa
Olivia E.
Pulcha-Llerena1, Sofía D. Vivanco-Hilario1, Wilter C.
Morales-García1 ![]() *
*
1Unidad de Posgrado de Ciencias de la Salud, Universidad Peruana Unión, Escuela de Posgrado. Lima, Perú.
Cite as: Pulcha-Llerena OE, Vivanco-Hilario SD, Morales-García WC. Nursing process for a patient with ectopic pregnancy in the Gynecology Department of a hospital in Arequipa. Multidisciplinar (Montevideo). 2024; 2:89. https://doi.org/10.62486/agmu202489
Submitted: 08-12-2023 Revised: 04-04-2024 Accepted: 07-08-2024 Published: 08-08-2024
Editor: Telmo
Raúl Aveiro-Róbalo ![]()
ABSTRACT
Introduction: ectopic Pregnancy is the implantation and subsequent development of the fertilized ovum outside the endometrial cavity, with greater prevalence in the uterine tubes. Tubal rupture and hemorrhage causes morbimortality and is considered a true medical emergency.
Objective: to elaborate the nursing care process oriented to a patient with ectopic pregnancy.
Method: this is a descriptive qualitative research work, with a single case design, aimed at a 35-year-old patient. The Nursing Care Process was used, applying Margory Gordon's functional patterns as an assessment instrument.
Results: 6 nursing diagnoses were identified, prioritizing the main diagnosis: acute pain r/c biological injury agent manifested by verbal expressions and VAS scale 10/8. Nursing interventions were applied with effective result achieving improvement with change score +2; before PC extrauterine pregnancy and Shock CR are still in the process of improvement.
Conclusions: the clinical manifestations of an ectopic pregnancy were identified in the patient; the complication risk factors were determined and the nursing role was described by applying preventive care in hypovolemic shock. Collaborative problems and risks were identified and addressed through the nursing interventions and activities included in the EAP for ectopic pregnancy, achieving better health status.
Keywords: Ectopic Pregnancy; Nursing Care Process.
RESUMEN
Introducción: el Embarazo Ectópico es la implantación y posterior desarrollo del óvulo fertilizado fuera de la cavidad endometrial, con mayor prevalencia en las trompas uterinas. La ruptura tubárica y la hemorragia ocasiona morbimortalidad y se considera una verdadera emergencia médica.
Objetivo: gestionar el proceso de atención de enfermería orientado a una paciente con Embarazo Ectópico.
Método: el presente trabajo de investigación es cualitativa de tipo descriptivo, con un diseño de caso único, dirigido a una paciente de 35 años, se utilizó el Proceso de Atención de Enfermería aplicando el como instrumento de valoración los patrones funcionales de Margory Gordon.
Resultados: se identificaron 6 diagnósticos de enfermería, priorizando el diagnóstico principal: dolor agudo r/c agente lesivo biológico manifestado por expresiones verbales y escala de EVA 10/8. Las intervenciones de enfermería se aplicaron con resultado eficaz logrando mejoría con puntuación de cambio +2; ante el PC embarazo extrauterino y RC de Shock aún están en proceso de mejoría.
Conclusiones: se logró identificar en la paciente las manifestaciones clínicas de un embarazo ectópico, se determinaron los factores de riesgo de complicación logrando describir el rol de enfermería aplicando lo cuidados preventivos en Shock Hipovolémico. Se identifico problemas y riesgos de colaboración que fueron atendidos mediante las intervenciones y actividades de enfermería plasmados en el PAE para embarazo ectópico, logrando mejor estado de salud.
Palabras clave: Embarazo Ectópico; Proceso de Atención de Enfermería.
INTRODUCTION
Ectopic pregnancy is the implantation and development of the fertilized egg outside the endometrial cavity (Huerta & Lopez, 2022a). Marion and Meeks (2012, as cited in Ruiz, 2019a) explain that ectopic pregnancy is defined as the implantation of the blastocyst outside the endometrium; 95 % is lodged in the uterine tubes, this being the most common; it can develop in other sites, such as the ovary or intra-abdominal. Morbimortality in patients with ectopic pregnancies is due to tubal rupture and intra-abdominal hemorrhage; it is one of the main obstetric emergencies that requires prompt action.
According to WHO, the main causes of mortality in pregnant patients are severe hemorrhage, postpartum infections, and hypertensive diseases of pregnancy. The causes shock is one of the leading causes of death in pregnant women up to 42 weeks after delivery (Marik & Weinmann, 2019a).
During the years 1998-2005, the most important causes of mortality in pregnant women in North America were hemorrhage with 2,5 %, due to ectopic pregnancy rupture, placenta previa, placenta accreta, retained postpartum debris, coagulopathy, uterine atony; pulmonary thromboembolism with 10,2 %; amniotic fluid embolism with 7,5 %; 12,3 % given by hypertensive complications; 10,7 % by hypertensive disease of pregnancy; 10,7 % by sepsis; 1,2 % complications of anesthesia; peripartum cardiomyopathy with 11,5 %; stroke correspond to 12,4 % (Pacagnella & Borovac-Pinheiro, 2019).
The incidence of ectopic pregnancies worldwide has increased to about 1 to 2 % of all confirmed pregnancies, about 75 % of deaths in ectopic pregnancies, and about 10 % of the deaths in ectopic pregnancies.
The first trimester and 9 % of all deaths are related to ectopic pregnancy. Therefore, it is considered a significant cause of mortality during pregnancy (Liang et al., 2019). According to Ccayanchira and Sicha (2022), it is estimated that 1,4 % of all pregnancies in the United States correspond to ectopic pregnancies.
There have not been many studies on ectopic pregnancy in Peru. The rate of ectopic pregnancy at the Hospital Nacional Docente Madre Niño San Bartolomé was 1 in 767 pregnancies; the Instituto Materno Perinatal indicates that it was 3,3 in 1000 pregnancies (Quispe, 2019).
Varma R et al. (2009, as cited in Mieles and Rosado, 2021a) agree that the clinical manifestations appear from week seven of gestation. Likewise, pain and bleeding are manifested by abnormal pregnancy growth and distension of the implantation site. The rupture of the tubal ectopic occurs around the ninth week of gestation; the clinical manifestations are hemodynamic compromise and peritoneal irritation, which trigger hypovolemic shock.
The main complication of ectopic pregnancy is hypovolemic shock, which is caused by the abundant loss of blood at the intra-abdominal level, causing deficiency of blood volume and hypoxia in the tissues as a consequence of alterations that affect the body's hemodynamics and can even lead to death (Chiguay, 2021a).
The treatment of first choice in complicated ectopic pregnancy is surgical, which suggests greater observation and emotional support due to the total or partial resection of the affected organ (Gasparri et al., 2018a). The goal of surgical treatment is the maximum preservation of reproductive function (Huerta & Lopez, 2022b). There is the treatment
Medical with Methotrexate for ectopic pregnancy with of ˂4 cm, no fetal cardiac activity, no signs of rupture, and with a β-hcg <5000 IU/ml (Garita & Alvarado, 2021a).
The nursing interventions and activities considered in the EAP for ectopic pregnancy are based on scientific knowledge aimed at addressing the clinical manifestations and risk factors of ectopic pregnancy. The patient under study was attended from the time she was admitted to emergency obstetrics and gynecology, with a history of previous ectopic pregnancy, making her reproductive condition high-risk. The PAE was applied by collecting data through Maryori Gordon's assessment, which provided the identification of six nursing diagnoses and prioritized: Acute pain r/c biological injurious agent manifested by verbal expressions and 10/8 VAS scale; likewise, extrauterine pregnancy was identified as a problem of baryon queue: PC, prioritizing the CR of Hypovolemic Shock.
Applying the scientific methodology of the PAE, adequate nursing care was provided, interventions were executed promptly and effectively, the proposed objectives were achieved, body hemodynamics were maintained, and the current critical health situation was reduced. The prioritization of activities determined the management of hypovolemic shock, ensuring a better prognosis and pending intentions in the recovery process (Carvajal & Sanchez-Herrera, 2018a).
The nursing professional focuses his work on human care based on the EAP, through which he diagnoses, plans, executes, and evaluates his actions. He also considers integrality, completeness, safety, and the continuity required by the care subject at different times and scenarios (Carvajal & Sanchez-Herrera, 2018b).
Iyer and Taptich (2008) and Naranjo-Hernandez et al. (2018) say the Nursing Care Process consists of five stages:
· Assessment: consists of collecting and organizing data concerning the person, family, and environment.
· Nursing diagnosis: it provides the basis for selecting interventions and/or nursing activities generated for the nursing assessment.
· Planning: this establishes the development of a plan to prevent, reduce, or correct problems, set outcomes, and provide nursing interventions.
· Execution: is the implementation of the planned care.
· Evaluation: is the contrast between what was planned and the patient's state of health and the expected results.
This study aimed to apply a protocol of ECP for the care of patients with ectopic pregnancy in the gynecological-obstetric emergency department, leading to avoiding complications using competent and quality care for the prompt recovery of the patient.
General Objective
Elaborate the nursing process for patients with Ectopic Pregnancy using NANDA taxonomies. NIC, NOC and AREA Model.
Specific Objectives
To assess the clinical manifestations of ectopic pregnancy in the patient.
To determine the risk factors for complications in ectopic pregnancy. Describe the role of nursing in the care of patients with ectopic pregnancy. Formulate a nursing care plan for patients with ectopic pregnancy, using NANDA taxonomy, NIC, NOC and Lynda Carpenito's Bifocal Model.
Theoretical Framework
Definition
Ectopic pregnancy is the implantation and subsequent development of the fertilized ovum outside the endometrial cavity (Huerta & Lopez, 2022c).
Ectopic pregnancy is considered to be a complicated condition due to its severity, which occurs when the blastocyst implants outside the endometrium of the uterine cavity and is one of the main obstetric emergencies that occurs during the first three months of pregnancy (Martinez et al., 2018).
Marion and Meeks (2012, as cited in Ruiz, 2019b) explain that ectopic pregnancy is defined as the implantation of the blastocyst outside the endometrium; 95 % is lodged in the uterine tubes, this being the most common; it can develop in other sites, such as the ovary or intra-abdominal. Morbimortality in patients with ectopic pregnancies is due to tubal rupture and intra-abdominal hemorrhage. Therefore, it is considered one of the main obstetric emergencies that demands adequate and immediate management.
During the years 1998-2005, the most important causes of mortality in pregnant women in North America were hemorrhage with 2,5 %, due to rupture of ectopic pregnancy, placenta previa, placenta accreta, retained postpartum debris, coagulopathy, uterine atony; pulmonary thromboembolism with 10,2 %; amniotic fluid embolism with 7,5 %; 12,3 % due to hypertensive complications; 10,7 % due to hypertensive disease of pregnancy; 10,7 % due to sepsis; 1,2 % due to complications of anesthesia; cardiomyopathy, cardiomyopathy of the uterus and the uterus.
Peripartum is 11,5 %, and stroke is 12,4 % (Pacagnella & Borovac-Pinheiro, 2019).
There have not been many studies on ectopic pregnancy in our country. The rate of ectopic pregnancy in the Hospital Nacional Docente Madre Niño San Bartolomé was 1 in 767 pregnancies; the Instituto Materno Perinatal indicates that it was 3,3 in 1000 pregnancies (Quispe, 2019).
The diagnosis of ectopic pregnancy should be rapid; this allows preserving the reproductive potential and the functionality of the tube. As for surgical treatment, by laparoscopic means, when they are diagnosed before there is a rupture of the tube, they are a safe alternative (Chinizaca, 2019a).
Pathophysiology
The trophoblast cells of ectopic pregnancy are similar to normal fetuses and secrete chorionic gonadotropin hormone (CGH), supported by the corpus luteum that releases estrogens and progesterone that cause the changes in the first phase of pregnancy. The evolution in the first weeks is normal because fertilization has been performed correctly, and implantation is pathological (Ruiz et al., 2019c).
Ectopic pregnancy is linked to risk factors that damage the tube and alter embryo transfer. These risk factors are tubal surgery, salpingitis, previous ectopic pregnancy, endometriosis, congenital tubal abnormalities, and adhesions secondary to surgical interventions on the uterus, ovary, and other pelvic or abdominal organs (Parra, 2019a).
The most common site of ectopic pregnancy is the tubal. The reason for the incorrect implantation is related to problems in the fallopian tube and the ovary due to early interruption in the migration of the fertilized egg without presenting the symptoms of an ectopic pregnancy. The pregnancy continues and usually arrives in the second or third month, where the implantation of the egg is observed in different locations (Mamani, 2018).
Classification and Location
Abnormal implantations can be extrauterine in the ovary, uterine tubes, abdominal cavity, peritoneum, or intrauterine at the level of the cervix (Ruiz et al., 2019d).
Ectopic pregnancies are classified according to their severity or according to the site of implantation of the zygote.
98,3 % of ectopic pregnancies are due to tubal pregnancy, followed by implantation in the ampullary, isthmic, fimbrial, and interstitial zones. 1,7 % of implantation occurs outside the uterine tube in the ovary, abdomen, and cervix (Bombilla, 2021).
As for the location of the ectopic pregnancy, it is located in frequency, according to Mieles and Rosado (2021b):
1. Fallopian tube: 98,3 %
2. Ampullary region: 79,6 %
3. Isthmus: 12,3
4. Fimbria: 6,2 %
5. Horn: 1,9 %
6. Ovary: 0,5 %.
7. Cervix: 0,15 %.
8. Abdomen: 0,03 %.
Clinical Manifestation
There are no pathognomonic symptoms of ectopic pregnancy; the symptoms that occur may be nonspecific, such as amenorrhea followed by hemorrhage; when there is a ruptured ectopic pregnancy, it is characterized by intense abdominal pain and signs of peritoneal irritability. When the patient is examined, she presents intense pain on vaginal examination, and a pelvic mass can be palpated at the adnexal level. In addition, the patient may be found with bleeding and the presence of anemia that may progress to hypovolemic shock (Morales, 2018).
The clinical manifestations depend on the severity of the fluid loss and the impact it has on the internal environment. Symptoms caused by hypovolemia are linked to reduced tissue perfusion. The earliest ones include lassitude, easy fatigue, thirst, cramps, and postural dizziness (Mieles & Rosado, 2021c).
The most common symptoms of ectopic pregnancy are given by a typical triad of abdominal pain, pelvic mass amenorrhea, and sometimes transvaginal bleeding. These symptoms are present in approximately 80 % of patients; the main symptom for which patients consult is pelvic pain. It should be noted that other presenting symptoms are abdominal hypersensitivity, adnexal hypersensitivity, pain mobilization of the cervix, uterine enlargement, fever, dizziness, and nausea (Hendriks, 2020a).
Varma R et al. (2009, as cited in Mieles and Rosado, 2021d) cite and agree that the clinical manifestations appear from seven weeks of gestation. Likewise, pain and bleeding are manifested by the abnormal growth of the pregnancy and distension of the site of its implantation. The rupture of the tubal ectopic is given around the ninth week of gestation.
Week of gestation manifests with hemodynamic risk and peritoneal irritation, which progresses to hypovolemic shock or when.
Risk Factors
They are strongly associated with pathologies that cause disorder within the standard fallopian tube conduction mechanism. The more tubal injury there is, the greater the risk of developing an ectopic pregnancy (Morales, 2018).
Risk factors include a history of pelvic inflammatory disease, smoking, fallopian tube surgery, previous ectopic pregnancy, and infertility (Hendriks, 2020c).
Ectopic pregnancy after natural ovulation and fertilization are associated with risk factors that injure the tube and alter embryo transport, such as previous tubal surgery, salpingitis, previous ectopic pregnancy, endometriosis, congenital tubal abnormalities and adhesions secondary to surgical interventions on the uterus, ovary and other pelvic or abdominal organs (Pincay, 2021).
Finally, we can say that the most common risk factors for developing an ectopic pregnancy are:
· Pelvic inflammatory disease.
· Use of the intrauterine device.
· Previous genital infections.
· Sexually infections, especially caused by chlamydia trachomatis.
· Previous tubal pregnancy.
· Congenital alterations (diverticula, atresic tubes, hypoplasias).
· Coitus before the age of 18 and promiscuity.
· Lower hemiabdomen surgery, which is caused by appendectomy or peritoneal adhesions.
· Assisted reproduction.
· Smoking, due to the toxicity nicotine on the tube.
· Maternal age.
Complications
Ectopic pregnancy with rupture causes hemorrhage that occurs gradually or rapidly, which can produce hypovolemic shock, and blood in the peritoneum eventually produces peritonitis. Therefore, it is considered that the first complication is hemorrhage, which leads to anemia, putting the pregnant woman's life at risk, and may lead to hysterectomy due to hypovolemic shock (Chiguay, 2021b).
Regarding abdominal ectopic pregnancy, complications such as peritonitis, pelvic abscess, and sepsis occur (Chiguay, 2021c).
According to Morales (2018), the most frequent complications of ectopic pregnancy are:
Hemorrhage is one of the first complications to occur.
Sepsis: due to the presence of trophoblastic debris at the implantation site.
Hypovolemic shock: it is caused by blood loss at the vaginal level, which causes a deficiency of circulating volume, and in turn, the oxygen in tissues and organs is diminished, which causes various internal alterations and can lead to death (Morales, 2018).
Acute abdomen, in gynecology, is the most common cause that is given by ectopic pregnancy, being of persistent location of tubal origin. (Morales, 2018).
On the other hand, fallopian tube rupture gives rise to hemorrhages in the abdominal cavity, as well as circulatory shock and collapse, anemia, hypovolemic shock, and sepsis (Bertin et al., 2019).
Therefore, hypovolemic shock is the consequence of different clinical or surgical conditions that will produce a rapid and significant loss of volume (hypovolemia), tissue perfusion deficit, and multiple organ failure (Kislitsina, 2019).
Diagnosis
The diagnosis of an ectopic pregnancy is based on transvaginal ultrasound and blood and urine analytical results of human chorionic gonadotropin (β-hCG). If the patient is in unstable condition, after clinical suspicion, by the presence of symptoms such as transvaginal bleeding, abdominal pain, unilateral pelvic pain and is associated with hemodynamic instability, the diagnosis is confirmed at the time of surgical exploration (Garita and Alvarado, 2021b).
Treatment
Treatment of ectopic pregnancy involves medical management with the use of intramuscular methotrexate, and surgical management through salpingostomy or salpingectomy. A patient presenting with peritoneal signs or hemodynamic instability should be admitted immediately for surgery (Hendriks, 2020d).
Patients with hemodynamic instability should be managed promptly and a good venous access should be sought with venocath N° 18 parenteral administration of crystalloids at rapid infusion. Finally, diuresis should be quantified at all times (Parra, 2019b).
Medical Treatment
It is the method used in preference by many physicians who seek to preserve the fertility of the patient, it is a treatment that is performed as long as the diagnosis is early and timely, therefore, it is indicated in hemodynamically stable women, with ectopic pregnancy of ˂4 cm, without fetal cardiac activity, without signs of rupture and with a β- hCG <5000 IU/ml (Garita and Alvarado, 2021c).
Methotrexate: It is an opposite of folic acid, interferes with DNA synthesis and cell multiplication. It has a high affinity for trophoblastic tissue, it acts by inhibiting its rapid cell proliferation, it is a tissue especially vulnerable to action of methotrexate, it so by inhibiting purines and pyramidines, which when not synthesized also affects DNA synthesis (Chinizaca, 2019b).
Methotrexate is a drug with strong side effects on somatic cells, .e. those with a rapid reproductive capacity. This drug has been used mainly for the treatment of ectopic pregnancies and malignant tumors. There are not many studies regarding the side effects of the drug on female reproductive cells (Tian et al., 2018).
Surgical Treatment
Surgical treatment is subject to the general condition of the patient, as well as her desire to become a mother and the situation of the tubal pregnancy. The method chosen for the surgical treatment is diagnostic laparoscopy with salpingostomy which aims to preserve the
Tubes. Laparotomy is indicated in hemodynamic instability because it allows rapid access to the pelvic structures (Gasparri et al., 2018b).
Salpingectomy consists of the partial or total removal of the damaged tube.
Salpingostomy is used to remove ectopic pregnancies of 2cm in length. An incision is made over the tube involved by the gestational sac, removing the contents causing the least damage to the tube; small hemorrhages are stopped by electrocautery. This technique is a good alternative since it is more conservative (Huerta & Lopez, 2022d).
Finally, it is mentioned that the treatment of the ectopic has always been surgical, and for a long time, salpingectomy was the intervention of choice. Laparoscopy has replaced laparotomy in terms of preserving fertility and the patient's desire to become a mother; linear salpingostomy has replaced salpingectomy as long as there is no extensive tubal damage (Alonzo et al.,2019).
Nursing Care in Ectopic Pregnancy
The intervention and/or nursing activities are based on scientific knowledge, specifying strategies for timely intervention using the NANDA, NIC, NOC taxonomy. This allowed making the best decision in favor of the user's stability and recovery (Melgarejo, 2018a).
Moltó (2022), describes the nursing care that should be provided to a patient with an ectopic pregnancy, and mentions the following:
· Assess pain and analgesia, if necessary.
· Control of bleeding: fluid replacement, monitor for signs of shock.
· Assess the state of consciousness, perfusion of skin and mucous membranes.
· Educate about the importance of keeping a menstrual cycle.
· Initiate obstetric emergency management.
· Look for signs of hypovolemia.
· Laboratory tests.
· Assess the type of treatment.
· Teaching relaxation techniques.
· Emotional management and support regarding what is going on.
Prevention
Ectopic pregnancies cannot be prevented, but here are some ways to decrease the risk:
· Smoking cessation.
· Limiting the number of sexual partners
· Using condoms during unsafe sex to help prevent sexually transmitted infections and may reduce the risk of pelvic inflammatory disease (Núñez, 2018).
· Finally, the control and prevention of risk factors that may lead to possible ectopic pregnancy should have periodic gynecological controls (Lizardo, 2021).
Acute Pain
It is the uncomfortable emotional and sensory experience related to actual or potential tissue damage, with unexpected or delayed onset of any intensity ranging from mild to severe.
Severe, with a premature or early end and lasting less than three months (Herdman and Kamitsuru, 2018a).
According to Torcal and Ventoso (2020a) the classification is as follows:
Acute Pain
It is a pain of short duration that is usually felt after illness, injury, surgery or childbirth. It soon responds to the administration of analgesia. If the duration exceeds 3 or 6 months it can be considered chronic (Torcal and Ventoso,2020b).
Chronic pain: it is pain that persists beyond what is normal for an acute disease (3 or 6 months) or after a reasonable healing time persists that does not disappear or that returns frequently. Examples: diabetic neuropathy, trigeminal neuralgia (Torcal and Ventoso, 2020c).
Nociceptive
Somatic: it is the one whose origin is the nociceptive information coming from any tissue that constitutes the structure of the body, produced by mechanical, thermal or chemical stimuli.
Visceral: it originates in the receptors of the viscera.
Neuropathic: it is the result of damage or direct injury to nerve structures or dysfunction of the peripheral or central nervous system. Described as unpleasant, burning, stabbing sensation.
Mixed: combination of more than one type of pain (Torcal and Ventoso, 2020d).
Acute pain is related to several causal factors, including chemical injury agents, injury by biological agents, and injury by physical agents (NANDA, 2020).
Acute pain is defined as an unpleasant sensory and emotional experience caused by actual or potential tissue injury, associated with tissue damage, with a sudden or slow onset of any intensity from mild to severe, an anticipated or foreseeable end, and a duration of less than 3 months (Herdman & Kamitsuru, 2018b).
The Nursing Interventions Classification (NIC) defines pain management as the relief of pain or decrease to a tolerance acceptable to the patient (Butcher et al., 2018a).
As Perez (2022) states: "Acute pain triggers certain avoidance or protective mechanisms, which may be accompanied by hyperreactivity of the autonomic nervous system, which the association of acute pain with anxiety and autonomic physical signs, such as pallor, sweating, vomiting, hypertension, tachycardia, among others manifests."
According to Murillo (2020a): "pain is a subjective experience, so it will be the patient himself who describes and verbally evaluates the intensity of the pain and the symptoms associated with it, and a comprehensive assessment of the pain using one of the pre-established scales such as the visual analog scale (VAS) that measures the intensity of pain is necessary."
Abdominal pain is a probable sign of the development of ectopic pregnancy; this type of pain is related to the development of the fetus in a smaller cavity than usual, which may be the fallopian tube; this executes pressure on the surrounding tissue, sending pain, signals to the mother. Pelvic pain is one of the most common symptoms, which is the reason for the
Which they attend the emergency. Approximately 95 % of women with tubal pregnancy present with pain in the pelvic and abdominal region (Berrios, 2019).
Therefore, the nursing assessment of an ectopic pregnancy should be focused on the clinical manifestations that occur, the main one being abdominal pain of the colicky type, which is one of the characteristic symptoms of the classic triad previously described; thus, the assessment of pain is of great importance within nursing activities, and the visual analog scale can be used as a tool (Murillo, 2020b).
Therefore, in the nursing care of a patient with ectopic pregnancy, it can be assessed that the most prominent problem is acute pain, both pre and post-surgical, so the action should be prompt and timely (De la Cruz, 2018).
Hypovolemic shock
Hypovolemic shock is the consequence of different clinical or surgical conditions that will result in rapid and significant volume loss (hypovolemia), tissue perfusion deficit, and multiple organ failure (Kislitsina, 2019).
Regardless of the cause, shock produces circulatory insufficiency so that the tissues receive an insufficient supply of glucose and oxygen; if it is not controlled, cell damage is irreversibly produced, resulting in cell death (Chiguay, 2021d).
According to WHO, the main causes of mortality in pregnant patients are severe bleeding, postpartum infections, and hypertensive diseases of pregnancy. Causes shock is one of the leading causes of death in pregnant women up to 42 weeks after delivery (Marik & Weinmann, 2019b).
The most frequent complication is hemorrhage, which leads to anemia and, subsequently, to hypovolemic shock, putting the patient's life at risk.
The complication that occurs in abdominal ectopic pregnancy is pelvic abscess, peritonitis, and sepsis due to the presence of trophoblastic debris (Chiguay, 2021e).
Therefore, hemorrhage is the leading cause of hypovolemic shock; it is also one of the most serious complications in obstetric patients and is considered the leading cause of maternal death, morbidity, and fetal mortality (Román & Quispe, 2019).
Castiblanco et al. (2022) define hypovolemic shock as the "syndrome that results in inadequate cell perfusion to maintain cell metabolism and occurs secondary to a sudden drop in circulating blood volume."
Alterations in the internal milieu produce the clinical manifestations of Hypovolemic Shock. They are caused by muscle weakness due to hypokalemia or hyperkalemia, polydipsia, and polyuria due to hyperglycemia or severe hyperkalemia and lethargy, confusion, convulsions or coma due to hyperglycemia, hyponatremia or hypernatremia. (Kislitsina, 2019).
Theoretical Model
For the present work, I consider Jean Watson and his Theory of Human Care. His theory enhances human care, taking into account that it is an activity proper to human beings, which has been practiced since primitive times and cannot be separated from human nature.
For Jean Watson, the success of caring is achieved through person-to-person support and the interactions generated by this process. Watson refers to caring as the moral reason for nursing (Riegel et al., 2018a).
Nursing care is manifested in interpersonal practice, which is intended to promote the health and growth of the individual and defines care as a process.
Between two people with their dimensions, feelings, emotions, and attitudes are involved, and commitments are acquired in caring (Henao, 2022).
Virginia Henderson's model was also considered, which is based on the satisfaction of basic human needs for life and health as a fundamental component of nursing care, considering the person as a whole being, with biological, psychological, sociocultural and spiritual dimensions, in continuous interaction, considering that the nurse's role is to help the healthy or sick person to preserve or recover their health has five essential phases that can be applied and used in the Nursing Care Process for patients with ectopic pregnancy (Melgarejo, 2018b).
The primary function of the nursing care process is to carry out work based on scientific evidence through critical and logical thinking, taking as a reference the different theories and their nursing models to offer standardized care in a holistic manner that contributes to the health and recovery of each individual (Fernández, 2022).
METHOD
Study Design
This is a qualitative, single clinical case study and the nursing care process (NCP) was as a method.
Study Subject
This is a 35-year-old female patient, who was admitted to the Obstetrics and Gynecology emergency room, accompanied by a family member and in a wheelchair. She reported that 2 days ago she presented cramp-like abdominal pain in the right lower quadrant, and also presented transvaginal bleeding 7 days ago.
of moderate quantity. Today she presented with nausea and vomiting. The patient reports being worried about her health; she a pained, tearful and fearful face.
She was diagnosed with complicated ectopic pregnancy and acute surgical abdomen and subsequently underwent an emergency exploratory laparotomy.
Scope and Period of Study
The present study was carried out in the gynecological-obstetric emergency service of a hospital in Arequipa, where the first data collection took place. The study period was carried out during the 12 hours of June 5th of the present year.
Information Gathering Procedure
Source of Information
The source of reference used was data collection, by interviewing the patient herself, another source was the clinical history and the nursing assessment according to Marjory Gordon's 11 patterns.
A bibliographic review of scientific evidence was also carried out in the following databases: Science, Scielo, Elsevier, Google Scholar.
Data Collection Technique
As a technique, the interview with the patient was used, being the main source and very useful to obtain information; likewise, the observation of the subject of the study was fundamental.
Information Procedure: information was collected in phases:
The First Phase: it began with a review of the patient's clinical history to obtain clinical data such as history, reasons for consultation, test results, etc. The first phase of the study began with a review of the patient's clinical history.
diagnostic tests, medical diagnosis, medical evolution, as well as the evolution of nursing care.
Second Phase: the nursing assessment began with a personal interview, using Marjory Gordon's 11 Functional Patterns, identifying the main nursing diagnoses for the elaboration of the specific care plan.
Third Phase: the two follow-ups performed on the patient were found to see the evolution of the patient.
Fourth Phase: a comprehensive analysis of the scientific evidence was carried out, limiting according to the date criteria, preferring to search for information from 2018 to the present. The following databases were used: Science, Scielo, Elsevier, Google Scholar and using keywords such as: nursing, nursing process, ectopic pregnancy.
Data Processing
The data were examined and organized based on the nursing approach.
First Moment
A prioritization network on the nursing methodology associated with the AREA Model (Pesut and Herdnan, 2019a) was performed with the assessment of the patient based on 11 functional patterns of Marjory Gordon, to select the primary diagnosis according the NANDA I taxonomy. Then, after the choice of the primary nursing diagnosis, we proceeded to the establishment of the expected outcomes criteria (NOC) and nursing interventions (NIC) and the respective activities.
Second Moment
A critical analysis of the scientific evidence included in this study was performed, taking as a basis the objectives raised according to NOC taxonomy (Moorhead et al., 2018) and prioritizing it with the AREA model (Pesut and Herdman, 2019b) to obtain the primary NOC of the Nursing Diagnosis and Primary Collaborative Problem and thus develop the care plan based on NIC taxonomy Butcher et al., 2018b).
Finally, the programmed nursing interventions and/or activities were carried out and then the evaluations of these activities were performed to check the extent of the interventions carried out according to the patient's individualized care plan.
RESULTS
Case Description
General Data
Patient G.Q.A., 35 years old, was admitted to the Obstetrics and Gynecology emergency room at approximately 10 am accompanied by a family member and in a wheelchair, communicative, manifesting abdominal pain in the right lower quadrant, cramp-like, 2 days ago, she also presented transvaginal bleeding 7 days ago of moderate amount. Today, she presents nausea and vomiting. The patient is worried about her health; she has a painful, pale, tearful, and fearful face.
Physical examination revealed a painful abdomen on palpation in the right iliac fossa. On medical examination, there was a pointed cervix, scanty dark bleeding, and on palpation, the uterus was painful on mobilization with palpation of a tumor in the right adnexa measuring approximately 5x4cm.
Personal History: denies allergies, blood group O+, sexual relations began 15 years ago, and contraceptive method 3 months ago.
She had the following surgical history: left salpingectomy for ectopic pregnancy 2 years ago and appendectomy 8 years ago.
Her current situation is as follows: communicative patient, on LOTEP, with Glaswon of 15, manifesting abdominal pain in the right lower quadrant, cramp type 2 days ago, presenting nausea and vomiting, concerned about her health status and the presence of vaginal bleeding, likewise the suspicion of being pregnant. Body weight is 65 kg, height is 1,55, and BMI is 27,05 (overweight).
Current Medical Diagnosis: acute Surgical Abdomen, complicated right ectopic pregnancy: Tubal rupture.
Medical Therapeutics:
· NPOClNa 9/oo 1000cc 45 drops Ranitidine 50mg EV single dose Metoclopramide 10mg EV single dose Dimenhydrinate 50mg EV single dose Cefazolin 1g 30 min before SOP Transfuse 2 globular pack Surgical preparation
· Surgical Irrigation
· Pre-surgical laboratory tests Gynecological ultrasound.
· Auxiliary examinations.
· BHCG 2560 UI/ML
· Pregnancy test (+) Results: Hemoglobin 7 g/dl
|
Table 1. Hemogram |
|
|
Leukocytes |
9.16 |
|
Abastonados |
0 |
|
Segmented |
58 |
|
Lymphocytes |
33 |
|
Monocytes |
0,8 |
|
Eosinophils |
0,1 |
|
Blood group and RH factor |
+ |
|
Platelets |
208 |
|
Glucose |
98 |
|
Creatinine |
0,76 |
|
TP |
13,8 |
|
TPT |
25,5 |
|
INR |
134 |
|
Sediment per field |
|
Leukocytes 8-12 x field Bacteria Positive Epithelial cells 4-6 x field Hematies 2-3 x field.
Immunologic
HIV Non-Reactive.
RPR Non-Reactive.
Ultrasound: free liquid is observed in moderate quantity, right ovary is found mixed tumor of 40x30mm.
Indications: Emergency exploratory laparotomy FC FC 118
PA 109/63 FR 22
T 36,3
S02,96 % FUM 11/4/22? FO G1P0A1
Assessment according to Functional Health Patterns Case Assessment
The assessment of the patient with a diagnosis of ectopic pregnancy is carried out with the application Maryori Gordon's 11 functional patterns.
Functional Pattern I: Perception and Control of Health
She is in fair health, received vaccination up to third dose of COVID 19 vaccine, operated 2 years ago for left salpinguectomy due to ectopic pregnancy and appendectomy 8 years ago. She is not allergic to drugs or food, she denies consuming tobacco and alcohol, in the last 2 days she self-medicated paracetamol every time she felt pain. She has a regular state of hygiene.
Functional Pattern II: Nutritional - Metabolic
· T: 36,0, Weight 65 kg, Height: 1,55, BMI 27,04 (overweight)
· Breathing: 22 rpm,
· Skin with moderate pallor, regular hydration status, with oral mucosa slightly moist and thirsty sensation. Skin intact, with scars of previous surgeries in the abdominal area.
· Oral cavity: complete dentition, oral mucosa without lesions, slightly moist and in a regular state of hygiene.
· Decreased appetite with nausea and vomiting (1 time) of food content, she has not been fed for approximately 18 hours.
· Distended abdomen, painful in the right iliac fossa.
· Leukocytes; 11 000
· Glucose: 98 mg/dl
· Hemoglobin. 7,0
Functional Pattern III: Elimination (Effective)
Adult patient, spontaneous urination. Urine sediment result. Leukocytes 8- 12 x field, bacteria +, epithelial cells 4-6 x field, red blood cells 2-3 x field.
Functional Pattern IV: Activity/Exercise (Effective)
Respiratory activity: the patient is ventilating spontaneously with FR: 22 x', Sat 96 %, pulmonary auscultation shows vesicular murmur present, no cramps or snoring.
Circulatory activity: she presents rhythmic heart sounds, with HR: 118 X', P/A 110/65, and capillary filling less than 2", likewise, there is no evidence of edema. With degree of dependence III.
Functional Pattern V: Effective Sleep-Rest
The patient reported sleeping only 6 hours because she was taking painkillers at night. She seems nervous, tearful and afraid. The patient reports that she cannot sleep very well due to the presence of constant abdominal pain for the last 2 days.
Functional Pattern VI: Cognitive-Perceptual (Altered)
The patient is awake in LOTEP, Glasgow 15, she is aware of her health problem, as she has previously gone through the same, she has a painful facial expression and refers intense abdominal pain, irritable and painful abdomen on palpation with more sensitivity in the right flank with evaluation 10/8 (severe pain) according to Eva scale. She is restless.
Functional Pattern VII: Self-perception-self-concept (Altered)
Nervous, tearful and fearful patient. She presents expressions of hopelessness: "She says I have no children yet, that worries me, because I have not been able to get pregnant, this is my second ectopic pregnancy".
Functional Pattern VIII: Role-Relationships (Effective)
Female adult patient, married, marital status, states: "I work in a beauty salon, I have been married for 5 years and I have no children yet, that worries me, because I have not been able to get pregnant, this is my second ectopic pregnancy, my husband supports me and worries about me".
Functional Pattern IX: Sexuality and Reproduction (Altered)
The married patient, who previously had a pregnancy that ended in ectopic pregnancy, currently does not refer with accuracy to the date of her last menstrual period, which would be 11/4/22. She used contraceptive methods, but 3 months ago, she stopped using them. The quantitative Beta test showed 2560 IU/ml. A transvaginal ultrasound found free liquid in moderate amounts on the right ovary with a mixed tumor of 40x30mm with slight vaginal bleeding. Ultrasound diagnosis: right ectopic pregnancy.
IRS: 18 years; Gestations: 1 Abortion: 1. Births: 0 MAC: 3 months ago Amenorrhea more or less than 2 months. Pregnancy test: positive Patient with scanty dark bleeding.
Soft breasts toco turgid, nipples formed without presence of secretion. Genitalia with presence of hematic discharge in moderate quantity.
Functional Pattern X: Adaptation Stress Tolerance (Altered)
Patient demonstrates concern for the condition of illness and hospitalization.
She is stressed upon learning of the ectopic pregnancy and expresses concern that she will no longer be able to have children.
Functional Pattern XI: Values and Beliefs (Effective)
Adult patient, of catholic religion and refers to having plans for the future.
Care Plan
Diagnostics
Nursing identification: the formulation of nursing diagnoses was developed using the NANDA I taxonomy (2021 - 2023).
Functional Pattern II: Nutritional-Metabolic
00205 Risk of shock evidenced by hypoxemia (Hemoglobin 7mg/dl).
Definition. Susceptible to inadequate blood flow to tissues that can lead to cellular dysfunction, which can compromise health (Heather and Kamitsuru, 2021a).
Domain 11: Safety and Security.
Class 2: Coping Responses.
00004 Risk of infection evidenced by increased pathogens in the environment, associated with anemia.
Definition. Susceptible to invasion and multiplication of pathogenic organisms, which may compromise health (Heather and Kamitsuru, 2021b).
Domain 11: Security measures.
Class 1:Infection.
Functional Pattern VI: Cognitive-Perceptual
00132 Acute pain r/c biological injury agent manifested by verbal expressions and VAS 10/8.Definition. "Unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage, of sudden or slow onset of any intensity from mild to severe with an anticipated or predictable end, and lasting less than 3 months" (Heather and Kamitsuru, 2021c).
Domain 12: Comfort.
Class 1: Physical Condition.
Functional Pattern VII: Self-perception - Self-concept
(00146) Anxiety related to pain and unsatisfied motherhood manifested by crying and expression of fear.
Definition. "Vague, uneasy feeling of discomfort or threat accompanied by an autonomic response (the source of which often nonspecific or unknown to the person); feeling of apprehension caused by anticipation of danger. It is a warning signal that warns of impending danger and enables the person to take action to deal with the threat." (Heather and Kamitsuru, 2021d).
Domain 9: coping/Stress Tolerance.
Class 2: coping Responses.
Functional Pattern IX: Sexuality and Reproduction
00221 Ineffective maternity process related to insufficient knowledge about the maternity process manifested by ineffective management of bothersome symptoms during pregnancy.
Definition. "Inability to prepare for and/or maintain a healthy pregnancy, birthing process, and newborn care to ensure the well-being of the newborn." (Heather and Kamitsuru, 2021e).
Domain 8: sexuality.Class 3: reproduction.
Functional Pattern X: Adaptive Stress Tolerance
00148 Fear Related to Unknown Situation.
Definition. A basic, intense emotional response that is aroused by the detection of an imminent threat, involving an immediate alarm reaction (Heather and Kamitsuru, 2021f).
Domain 9: coping / Stress Tolerance.
Class 2: coping responses 33.
Prioritization of the Principal Nursing Diagnosis, using a critical reasoning network based on the AREA Model
Principal Diagnosis
Diagnosis of Principal Nursing (DxEp)
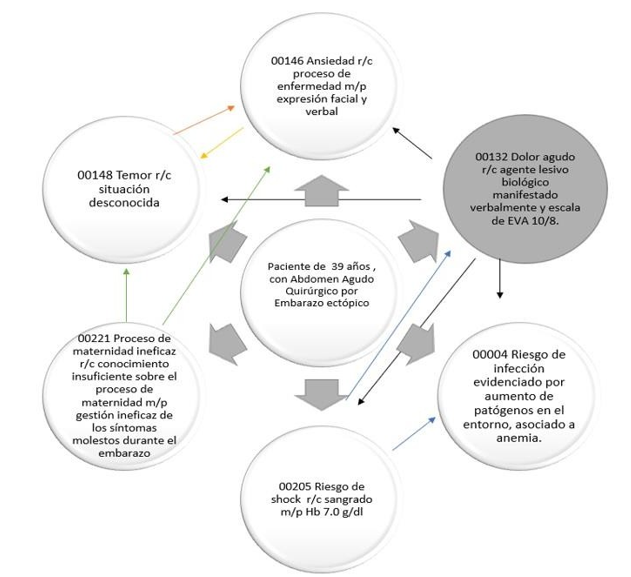
According to the AREA Reasoning Network, the interrelation of the altered diagnoses (figure 1) is obtained as DxEp:
· 00132 Acute pain related to biological agent injury expressed verbally and VAS 10/8.
· Definition. "Unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage, of sudden or slow onset of any intensity from mild to severe with an anticipated or predictable end, and lasting less than 3 months." (Herdman and Kamitsuru, 2021c).
· Domain: 12 Comfort.
· Class: 1 Physical comfort.
Figure 1. Critical reasoning network based on the AREA model, for obtaining the principal nursing diagnosis
Justification of the DxEp.
Acute Pain: pain of short duration that is usually felt after illness, injury, surgery or childbirth. The prompt response to the administration of analgesia. If the duration exceeds 3 or 6 months it can be considered chronic (Torcal and Ventoso, 2020e).
As Perez (2022) states, "Acute pain sets in motion certain avoidance or protective mechanisms, which may be accompanied by hyperreactivity of the autonomic nervous system, which the association of acute pain with anxiety and autonomic physical signs, such as pallor, sweating, vomiting, hypertension, tachycardia, among others manifests."
Pelvic pain is one of the most common symptoms, which is why they go to the emergency department. Approximately 95 % of women with tubal pregnancy present pain in the pelvic and abdominal region (Berrios, 2019).
Acute pain is transient and short-duration and is caused by an adverse stimulus associated with an acute illness, trauma, or surgery. It disappears when the origin is corrected. The accompanying manifestations are tachycardia, polypnea, and sweating. It is important to know the etiology of the pain and its duration. According to its characteristics, we can classify it as mild, moderate, or severe (Cabo de Villa et al., 2020).
According to the NANDA definition for acute pain, "Unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage, of sudden or slow onset of any intensity from mild to severe with an anticipated or predictable end, and lasting less than 3 months." (Herdman and Kamitsuru, 2021d).
According to Murillo (2020), for pain control, assessed through the VAS scale, "the following actions should be considered in practice: administration of an effective treatment for acute pain, facilitating safety by avoiding complications of the process, maintaining physical and psychological functionality, improving the quality of life within the possibilities of each individual, educating and guiding both the patient and the family in self-care and participation."
Abdominal pain in ectopic pregnancy occurs suddenly, intensely, and unilaterally and can be detected in 90 % of symptomatic cases, presenting palpatory tenderness and rebound signs, especially in complicated ectopic pregnancy (Berrios, 2019).
According to Vernaza et al. (2019), For the realization of an adequate diagnosis, the severity of the pain must be assessed. Therefore, the assessment and management of pain are of much.
The lack of control of the disease causes emotional and cognitive alterations in the patients.
According to Ramos et al. (2018), "Pain management and control are important to improve the person's quality of life; inadequate pain management would affect recovery."
The nursing assessment of an ectopic pregnancy should be focused on the clinical manifestations that occur, the main one being abdominal pain of the colicky type, which is one of the characteristic symptoms of the classic triad previously described; thus, the assessment of pain is of great importance within the nursing activities, and the visual analog scale can be used as a tool (Murillo, 2020).
Acute pain at high levels can aggravate the lived experience; they are very unpleasant experiences that manifest with physical and emotional alterations. They are physiological responses associated with trauma. The objective of our attention is to achieve the most excellent well-being and minimum effect of complications through analgesia, to calm the physical suffering, to manage the rest of the problems, and to continue with the assessment and observation of pain manifestations.
Prioritization of the Major Complication Risk, using a critical reasoning network based on the AREA Model
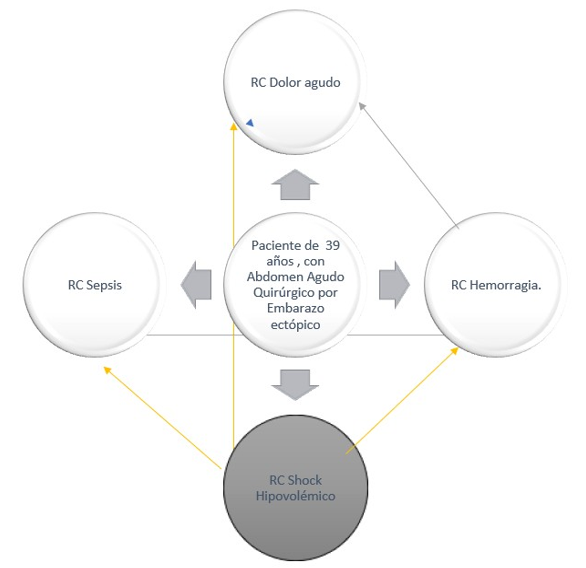
Figure 2. Critical reasoning network based on the AREA model, to obtain the main complication risk
Identification of the main CR
To determine the main CR, the interrelation of the four complication risks for the case of ectopic pregnancy was performed, with the Risk of Complication Hypovolemic Shock being one with the most interrelations according to Figure 2.
Identification of collaborative problems (CP) and their complication risks (CR)
In order to know which are the collaborative problems and complication risks that the patient may present during the hospital stay, we worked with Lynda Carpenito's Manual of Nursing Diagnoses.
Collaborative Problems
Extrauterine Pregnancy.
Complication Risks
RC Acute Pain. RC Hemorrhage.
RC Hypovolemic Shock. RC Sepsis.
Hypovolemic shock
It is the rapid loss of fluid that causes multiorgan failure due to inadequate circulation due to hypovolemia and subsequent inadequate perfusion; most commonly, this is due to rapid blood loss due to traumatic, medical, or surgical nature (Carpenito, 2021).
Hypovolemic shock is the consequence of different clinical or surgical conditions that will produce a rapid and significant loss of volume (hypovolemia), tissue perfusion deficit, and multiple organ failure (Kislitsina, 2019).
Hemorrhage is the loss of 500 or more of blood volume or bleeding that occurs at a rate greater than 150 ml/minute; therefore, it is the loss of 50 % of blood volume in 20 minutes (Carrillo et al., 2018).
The ruptured ectopic pregnancy causes hemorrhage that occurs gradually or rapidly, which can produce hypovolemic shock, and the blood in the peritoneum eventually produces peritonitis. Therefore, it is considered that the first complication is hemorrhage, which leads to anemia, putting the pregnant woman's life at risk, and may lead to hysterectomy due to hypovolemic shock (Chiguay, 2021).
Diagnosis of hypovolemic shock is more difficult when the source of blood loss is not visible.
Hypovolemic shock is easily diagnosed when there are signs of hemodynamic instability. In this sense, any patient of childbearing age with signs of shock should be tested to rule out pregnancy; its negativity rules out ectopic pregnancy as a cause of hypovolemic shock (Cannon, 2018).
The symptoms of hypovolemic shock depend on the intensity, the type of fluid lost, and the repercussions on the internal environment. In principle, the symptoms induced by hypovolemia are related to the decrease in tissue perfusion (Mieles, 2021).
The clinical manifestations of Hypovolemic Shock are produced by alterations of the internal milieu: muscle weakness due to hypokalemia or hyperkalemia, polydipsia, and polyuria due to hyperglycemia or severe hyperkalemia, lethargy, confusion, convulsions, or coma due to hyperglycemia, hyponatremia, or hypernatremia (Kislitsina, 2019).
A drop in hematocrit without a history of anemia suggests hypovolemia due to blood, even if there is no visible bleeding; causes of shock with hypovolemia respond well to vascular volume replacement and should be identified promptly (Mieles, 2021).
On the other hand, fallopian tube rupture gives rise to hemorrhages in the abdominal cavity, as well as circulatory shock and collapse, anemia, hypovolemic shock, and sepsis (Bertin et al., 2019).
To conclude, hypovolemic shock is the consequence of different clinical or surgical conditions that will produce a rapid and significant loss of volume (hypovolemia), tissue perfusion, and multiple organ failure (Kislitsina, 2019).
Finally, the main complication risk, hypovolemic shock, is presented in the patient with a hemoglobin of 7 mg/dl, for which she received three globular packages, considering hemorrhage a complication. The constant observation of signs and
Early symptoms of hypovolemia allowed collaborative interventions to restore physiological stability in the patient.
Planning
DxEp planning
For the main nursing diagnosis, the Nursing Outcomes Classification (NOC) literature of Moorhead et al., (2018) and the Nursing Interventions Classification (NIC) Butcher et al., (2018) were used for the purpose of measuring health outcomes and applying individualized nursing activity respectively.
DxEp
(00132) Acute pain r/c biological injury agent manifested by verbal expressions and VAS scale 10/8.
Definition: "Unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage, of sudden or slow onset of any intensity from mild to severe with an anticipated or predictable end, and lasting less than 3 months." (Herdman and Kamitsuru, 2021e).
Domain 12: Comfort.
Class 1: Physical Condition.
DxEp NOC Outcomes
As for DxEp (00132) Acute pain, it has the following NOCs:
· 2102 Pain level 1605 Pain Control.
· 3014 Patient Satisfaction 2109 Level of discomfort.
Prioritization of the NOC of the DxEp, using the critical reasoning network based on the AREA Model
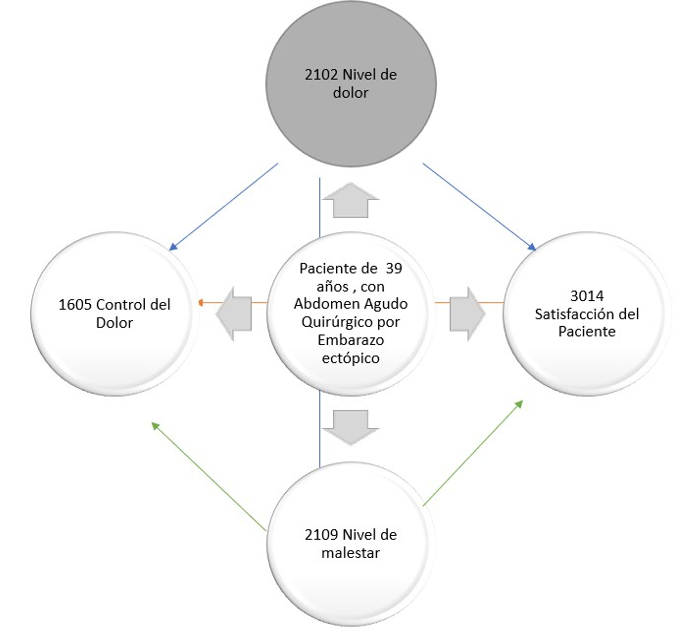
Figure 3. Prioritization of the NOC of the main diagnosis by means of a critical reasoning network based on the AREA model
DxEp Main NOC Rationale
After interrelating the NOCs, the one with the highest interrelationship:
· 2102 Pain level.
· Definition: "Intensity of referred or manifested pain." (Moorhead et al.,2018).
· Domain V: perceived health.
· Class V: symptomatology.
Murillo (2020) quotes Guevara et al. (2005), "Pain is an unpleasant experience associated with actual or potential tissue damage." The practical parameters of the VAS scale acute management are taken into consideration.
Acute pain is transient, short-duration, and caused by an adverse stimulus. It disappears when the origin is corrected. The accompanying manifestations are tachycardia, polypnea, and sweating (Cabo de Villa et al., 2020).
The evaluation of pain is subjective, and pain scales help. Observation is important so that relevant data can be collected to provide timely and effective care (Ccayanchira, 2022).
According to Murillo (2020), for pain management, assessed with the VAS scale, the following actions should be considered in practice: administration of an effective treatment for acute pain, facilitating safety by avoiding the complications of the process, maintaining physical and psychological functionality, improving the quality of life within the possibilities of each individual, educating and guiding both the patient and the family in self-care and participation.
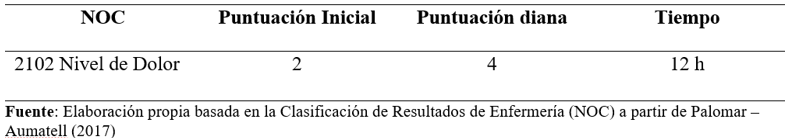
Figure 4. Main CR NOC score for DxEP
The figure 4 shows that the Pain Level outcome was assessed with an initial pain score of 2 (substantial) and after performing the interventions, a target score of 4 (mild) is expected to be achieved
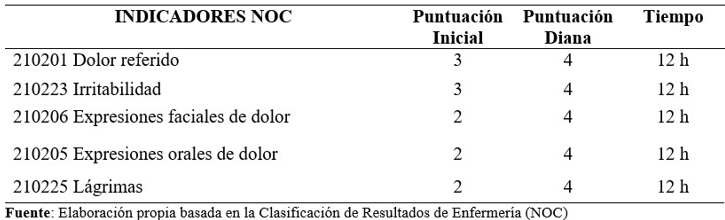
Figure 5. Scoring of NOC indicators of the main CR
The figure 5 shows that the Pain Level outcome was assessed with an initial pain score of 2 (substantial) and after performing the interventions, a target score of 4 (mild) is expected to be achieved.
DxEP INTERVENTIONS (IAS)
Interventions were obtained from the Interventions Manual (NIC): Butcher et al, 2018.
IAS 2210 Administration of analgesics:
· Definition: "Use of pharmacologic agents to decrease or eliminate pain." (Butcher et al., 2018).
· Field 2: physiological: Class H complex drug control activities.
· 221001 Determine the location, characteristics, quality, and severity of pain before placing analgesia on the patient.
· 221002 Verify the medical indications regarding the medication, dosage and frequency of the prescribed analgesic.
· 221003 Attend to comfort needs and other activities that aid in relaxation to facilitate response to analgesia.
· 221004 Evidence analgesic response and any adverse effects.
NIC 1400 Pain management
· Definition: "Relief of pain or decrease in pain to a level of tolerance that is acceptable to the patient." (Butcher et al., 2018)
· Field 1: physiological: basic.
· Class E: promotion of physical comfort.
Activities
140001 Conduct an assessment of pain including location, characteristics, duration, frequency, intensity.
140002 Examine nonverbal cues to pain.
140003 Ensure that the patient receives appropriate analgesic care.
140004 Use pain control measures before pain becomes severe.
NIC 2314 Administration of medication: intravenous (i.v.)
Definition: "Preparation and administration of medications intravenously." (Butcher et al., 2018)
Field 2: physiological.
Class H: complex drug control activities:
· 231401 Follow the five rules of proper medication administration.
· 231402 Take note of patient's medical and allergy history.
· 231403 Verify placement and patency of i.v. catheter in vein.
· 231404 Administer i.v. medication at appropriate rate.
Main CR planning
The objectives were extracted from the NOC: manual by Moorhead et al., (2018) and for the NIC interventions Butcher et al., (2018).
As a major complication risk: Hypovolemic shock.
NOCp results of the RC
NOC taxonomy is used to choose the RC for Hypovolemic Shock: 0419 Severity of shock: hypovolemic.
· 0401 Circulatory status.
· 0416 Tissue perfusion: cellular.
· 0413 Severity blood loss.
Prioritization of the Main RC NOC using Critical Reasoning Network based on the AREA model
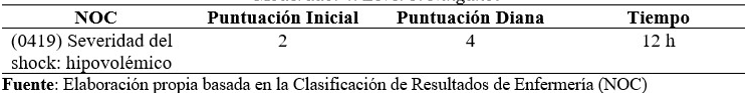
Figure 6. Main CR NOC score, according to Likert scale
Figure 6 shows us that for the outcome Shock Severity: Hypovolemic was assessed with initial score of 2 (substantial) and after performing the interventions and/or nursing activities, a target score of 4 (mild) is expected to be achieved.
Justification of the main NOC of the main CR. Prioritized NOC of CR Hypovolemic shock
(0419) Severity of shock: hypovolemic.
Definition: "Severity of signs and symptoms of inadequate blood flow for tissue perfusion due to a sharp decrease in intravascular fluid volume." (Moorhead et al.,2018).
Domain II: physiological Health.
Class E: cardiopulmonary.
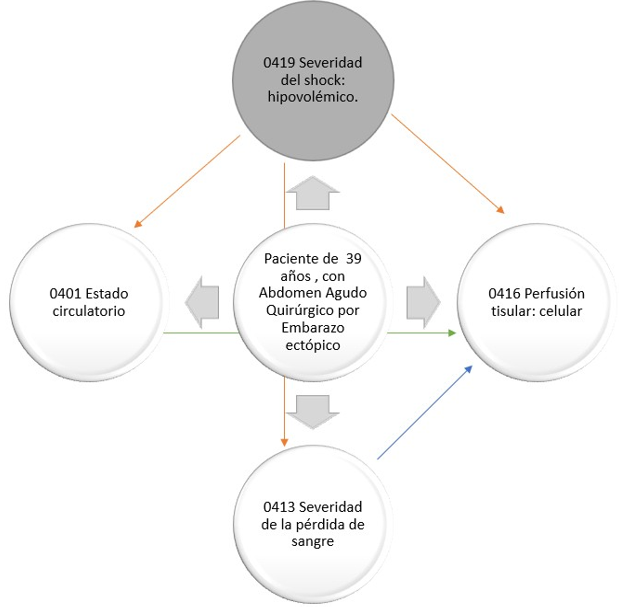
Figure 7. Prioritization of the NOC of the RCp by means of a critical reasoning network based on the AREA model
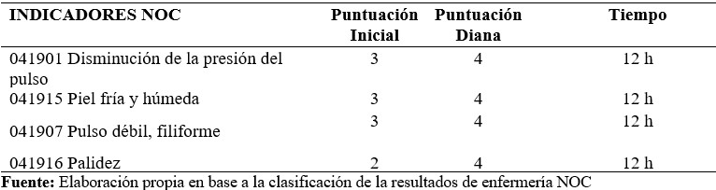
Figure 8. Scoring of NOCp indicators of the main CR, according to Likert scale
NIC interventions of the main CR
Interventions were taken from the Interventions Manual (IAS): Butcher et al, (2018).
IAS 6680 Monitoring of vital signs
Definition: "Collection and analysis of cardiovascular, respiratory, and body temperature status data to determine and prevent complications." (Butcher et al., 2018).
Field 4: security.
Class U: crisis management.
668001 Monitor blood pressure, pulse, temperature and respiratory status, as appropriate.
668002 Monitor respiratory rate and rhythm (depth and symmetry).
668003 Identify possible causes for changes in vital signs.
668004 Monitor and record for signs and symptoms of hypothermia and hyperthermia.
NIC 4170 Hypovolemia management
Definition: "Decrease in extracellular and/or intracellular fluid volume and prevention of complications in a patient with fluid overload." (Butcher et al., 2018).
Domain 2: physiological: complex.
Class N: control of tissue perfusion.
Activities
· 417001 Observe for sources of fluid loss (e.g., hemorrhage, vomiting, diaphoresis, and tachypnea).
· 417002 Preserve patent IV access.
· 417003 Administer prescribed parenteral solutions (e.g., saline).
· 417004 Position the patient in such a way as to promote peripheral perfusion.
IAS 4260 Prevention of shock
Definition: "Detection and treatment of a patient at risk of imminent shock." (Butcher et al., 2018).
Physiological domain 2. Physiological: Class N complex Control of tissue perfusion.
426001 Cannulate and maintain a large bore i.v. line, as appropriate.
426002 Administer i.v. fluids while monitoring hemodynamic pressures and diuresis.
426003 Administer oxygen and/or mechanical ventilation, as appropriate.
426004 Verify laboratory values, especially Hb and Hct levels, coagulation profile, arterial blood gases and electrolytes.
Finally, all the interventions and nursing activities that were planned were carried out during 12 hours, where all the proposed interventions could be executed, achieving hemodynamic stabilization of patient, likewise the patient is in the process of improvement after the adequate and effective administration of the interventions and/or nursing activities, achieving an improvement in a period of 12 hours.
Execution
The implementation of nursing interventions according to the prioritized diagnoses used the Classification of Nursing Interventions (Butcher et al., 2018).
|
Table 2. Timeline of nursing interventions/activities in ectopic pregnancy |
||||
|
Date |
Interventions / activities |
Shift |
||
|
|
DxEp interventions: |
M |
T |
N |
|
5 06 2022 |
NIC 2210 Administration of analgesics |
|
|
|
|
Activities: |
|
|
|
|
|
Determine the location, characteristics, quality and severity of the pain before placing the patient on analgesia. |
10 |
2 |
8 |
|
|
Verify the medical indications regarding the medication, dosage and frequency of the prescribed analgesic. |
11 |
|
|
|
|
Attend to comfort needs and other activities that aid in relaxation to facilitate response to analgesia. |
10 |
2 |
8 |
|
|
Evidencing analgesic response and any adverse effects. |
10 |
2 |
8 |
|
|
5 06 2022 |
NIC 1400 Pain management |
|
|
|
|
Conduct an assessment of pain including location, characteristics, duration, frequency, intensity. |
10 |
2 |
8 |
|
|
Examine nonverbal cues of pain. |
10 |
|
8 |
|
|
Ensure that the patient receives appropriate analgesic care. |
10 |
2 |
8 |
|
|
Use pain control measures before pain becomes severe. |
10 |
|
10 |
|
|
5 06 2022 |
NIC 2314 Medication administration: intravenous (i.v.) |
|
|
|
|
Follow the five rules of proper medication administration. |
10 |
2 |
8 |
|
|
Take note of the patient's medical and allergy history. |
10 |
|
|
|
|
Verify placement and patency of the IV catheter in the vein. |
10 |
|
|
|
|
|
Administer i.v. medication at the appropriate rate. |
10 |
2 |
8 |
|
|
RCp interventions: |
|
|
|
|
5 06 2022 |
IAS 6680 Monitoring of vital signs |
|
|
|
|
Monitor blood pressure, pulse, temperature and respiratory status, as appropriate. |
10 |
2 |
8 |
|
|
Monitor respiratory rate and rhythm (depth and symmetry). |
10 |
|
10 |
|
|
possible causes of changes in vital signs. |
10 |
|
10 |
|
|
Monitor and record for signs and symptoms of hypothermia and hyperthermia. |
10 |
|
10 |
|
|
5 06 2022 |
NIC 4170 Hypovolemia management |
|
|
|
|
Observe sources of fluid loss (e.g., hemorrhage, vomiting, diaphoresis, and tachypnea). |
10 |
|
|
|
|
To preserve a permeable i.v. access. |
10 |
|
|
|
|
Administer prescribed parenteral solutions (e.g., saline). |
10 |
2 |
8 |
|
|
Position the patient to promote peripheral perfusion. |
10 |
2 |
8 |
|
|
5 06 2022 |
IAS 4260 Prevention of shock |
|
|
|
|
Cannulate and maintain a large bore I.V. line, as appropriate. |
10 |
|
|
|
|
Administer i.v. fluids while monitoring hemodynamic pressures and diuresis, as appropriate. |
10 |
2 |
8 |
|
|
Administer oxygen and/or mechanical ventilation, as appropriate. |
10 |
|
|
|
|
Verify laboratory values, especially Hb and Hct levels, coagulation profile, arterial blood gases and electrolytes. |
10 |
|
10 |
|
Evaluation
It was carried out based on the evaluation of the pregnant woman's condition upon admission to the Obstetrics and Gynecology Emergency Room, after the administration of the main nursing activities and interventions, about the activities of the NOC of the DxEp: Pain Level and the NOC of the RCp: Hypovolemic Shock. In 12 hours of care, a slight improvement and stability of vital functions were achieved, obtaining a score of change+ 2.
The patient was observed to have a favorable evolution after the diagnosis of complicated ectopic pregnancy, improving acute pain and significantly reducing the risk of hemorrhage. Finally, it is concluded that the planned activities were practical in the planned results.
Evaluation of the DxEp DxEp result
00132 Acute pain r/c biological injury agent manifested by verbal expressions and VAS scale 10/8.
Definition: "Unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage, of sudden or slow onset of any intensity from mild to severe with an anticipated or predictable end, and lasting less than 3 months." (Herdman and Kamitsuru, 2021f).
Domain 12: comfort.
Class 1: physical condition.
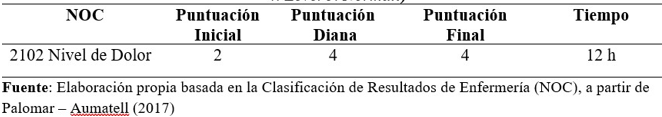
Figure 9. DxEp Main NOC score
The NOC pain level presented an initial score of 2 (substantial) after the application of the interventions and activities carried out, a final score of 4 (mild) was achieved.
The score obtained in the NOCp of the DXEp is 4 (mild) during the 12 hours. The pain has been decreasing since admission to the Obstetric Gynecological Emergency, therefore, the was achieved, observing a relieved facial expression and reporting a VAS of 10/3.
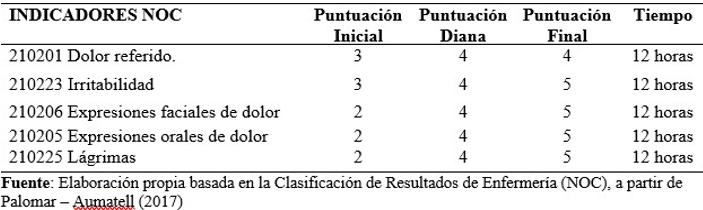
Figure 10. Scoring of NOCp indicators of the DxEp
In figure 10 in relation to the indicator (210201) referred pain, it can be seen that the patient presented an initial score of 3 (Moderate), after providing care and administration of parenteral analgesia (medical indication) the patient managed to achieve an improvement, achieving a final score of 4 (light) in 12 hours.
Regarding the indicator (210223) Irritability, which is significantly caused by acute pain, it started with a score of 3 (Moderate). It reached a final score of 5 (No pain) in 12 hours because the patient became calmer and less irritable as the pain decreased.
In relation to the indicator (210206) Facial expressions of pain, she presented an initial score of 2 (Substantial). When reducing the level of pain, the patient managed to reach a final score of 5 (no pain), observing a positive facial expression after the care provided.
As for the indicator (210205) Oral expressions of pain, as in the previous indicators, the result was achieved, starting with a score of 3 (Moderate) and reaching a score of 5 (No pain). This was also obtained by reducing the level of pain.
Finally, the indicator (210225) Tears obtained an initial score of 3 (Moderate) and reached a final score of 5 (No pain); therefore, the result has been achieved.
Evaluation of the Main RC Result
2102 Pain Level.
Definition. "Intensity of referred or manifested pain." (Moorhead et al.,2018).
Domain V: perceived health.
Class V: symptomatology.
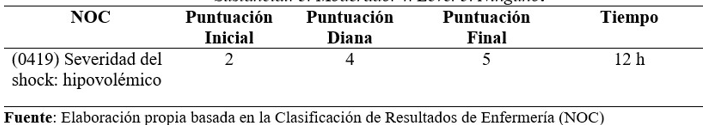
Figure 11. Evaluation of the NOC score of the main CR, according to Likert Scale
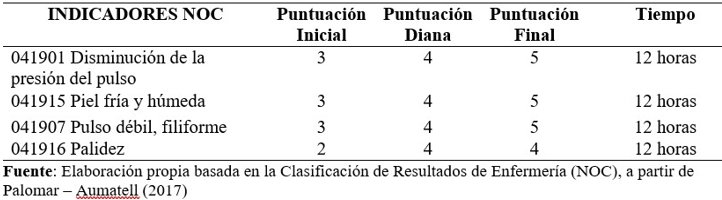
Figure 12. NOCp score of the main complication risk according to Likert scale.
Figure 11 shows us that for the NOC Severity of shock: Hypovolemic was assessed with an initial pain score: 2 (Substantial) and after performing the nursing interventions, a final score of 5 (None) was achieved.
In figure 12, regarding the indicator (041901) Decrease in pulse pressure, an initial score of 3 (Moderate) can be observed after the preventive nursing interventions, and a final score of 5 (None) is achieved during a 12-hour period.
Concerning the indicator (041915) Cold and moist skin, an initial score of 3 (moderate) was obtained; during the 12 hours, a final score of 5 (none) was reached.
About the indicator (041907) Weak pulse, thready: the initial score was 3 (Moderate); during the 12 hours, a final score of 5 (None) was obtained. Therefore, the result was achieved.
The indicator (041916) Pallor has an initial score of 2 (Substantial), and a final score of 4 (Mild) was obtained, not reaching the score of 5 (None) because the patient continues with pallor due to the presence of anemia.
Finally, the indicator (041922) Lethargy started with a score of 4, and at the end of 12 hours, a score of 5 was achieved, which is higher than the proposed target score.
Therefore, it can be concluded that thanks to the nursing activities and interventions and indicated treatment, hypovolemic shock was controlled in the patient.
DISCUSSION
The patient in this study was admitted to the Obstetrics and Gynecology Emergency Department to be seen for severe abdominal pain, presenting ectopic pregnancy, and CR of hemorrhagic shock, representing her current health problem.
Following the literature review, research has been obtained that exposes nursing interventions to patients with a diagnosis of ectopic pregnancy, according to Matos et al. (2018). Ectopic pregnancy with rupture causes bleeding that occurs gradually or rapidly and can trigger hemorrhagic shock. Finally, the peritoneal blood produces peritonitis. Therefore, it is considered that the first complication is hemorrhage, which leads to anemia, putting the pregnant woman's life at risk, and depending on the complication and intervention, it can lead to hysterectomy due to hypovolemic shock.
Through the PAE, the assessment and identification of the patient's needs were achieved. During this process, the interaction of the nurse with the patient herself is highlighted, which helps to mutually identify the needs and plan actions in search of strategies for coping with the current problem (Mejía, 2018).
The elaboration and execution of the nursing care plan allow the assessment of specific situations, the proposal of nursing diagnoses, the planning of interventions and activities related to the problem, the implementation of these interventions, and the evaluation of the results obtained (Moltó, 2022a).
It is important to perform a good nursing assessment to avoid risks of complications and some sequelae with irreversible damage to the patient. Nursing care with scientific knowledge allows holistic care to achieve an improvement in the health situation and incorporate it into family and society (Riegel et al., 2018b).
For Watson, the goal of nursing care is achieved through person-to-person support (Riegel et al., 2018c).
Watson's theory of human caring represents a moral and ethical professional commitment, which is essential in the care process. This process is based on a humanistic approach and, in turn, shows a deep interest in the person (Figueredo et al., 2019a).
Nursing care is based on scientific knowledge and uses appropriate intervention strategies, such as NANDA taxonomy, NIC, NOC, and Lynda Juall Carpenito's BIFOCAL Model, to make the best decision for the user's stability and recovery (Melgarejo, 2018c).
The DxEp acute pain was prioritized because the study patient referred an Eva of 10/8, manifested by facial expressions of pain, tears, and verbal. Herdman and Kamitsuru (2018g) tell us that pain is an uncomfortable emotional and sensory experience related to actual or potential tissue damage. With this concept in mind, the primary focus is reducing the pain level to address the underlying problem.
The CR of hypovolemic shock is a complication of ectopic pregnancy that is a cause of maternal morbidity and mortality. Interventions and/or nursing activities should be aimed at avoiding this type of problem. The patient under study presented bleeding and whose hemoglobin control was at 7mg/dl, which determined the transfusion of three globular packages before and after the surgical intervention. As mentioned by Morales (2018), anemia leads to hypovolemic shock abruptly and uncontrollably, which requires immediate action through the identification of signs and symptoms as part of the physical examination and manifestations of severe pain.
Limitations
During the elaboration of the nursing care process, some non-relevant limitations have been found to continue providing the nursing care that was applied in the first 12 hours, the following:
There was no interview of family members for the extension of data collection due to the restriction on visits due to the COVID-19 pandemic.
Analysis in the search for diagnoses and appropriate interventions for the pathology because the NOC does not include the diagnosis of ectopic pregnancy.
No permanent follow-up of the patient on subsequent shifts due to the rotating shift schedule on the workday.
CONCLUSIONS
Nursing was developed using the NANDA taxonomy, NIC, NOC, and AREA model to provide specific and priority care in the case of Ectopic Pregnancy.
The clinical manifestations of ectopic pregnancy were assessed in the patient by collecting signs and symptoms using Maryori Gordon's 11 functional patterns, taking into account Jean Watson's theory of humanized care and Virginia Henderson's theory of satisfaction of basic human needs for life and health, since it considers the person as a whole being, with biological, psychological, sociocultural and spiritual dimensions, which are in continuous correlation.
After the critical analysis of the data collected and the theoretical confrontation, risk factors in Ectopic Pregnancy were determined in the patient, establishing as a risk of complication: Hypovolemic Shock, which during the intervention process has been assessed, monitored, controlled, and documented.
After establishing the DxEp: Acute Pain and the RCp of Hypovolemic Shock, the results and interventions that define the importance of the nursing role in the care of patients with ectopic pregnancy were described, taking into account the research, the feasibility of the intervention, and the profile of the nursing professional.
Once the DxEp and Rcp interventions that aim to solve the needs and/or reduce the severity of the patient's health risk have been prioritized, a Nursing Care Plan is formulated for the single clinical case of Ectopic Pregnancy, applying the NANDA, NIC, NOC taxonomy and Lynda Carpenito's Bifocal Model. Subsequently, the plan is evaluated as an axis for improving interventions.
BIBLIOGRAPHIC REFERENCES
1. Alonzo, S. E. O., Blanco, F. V. y Saldaña, D. D. C. G. (2019). PREM de Ginecología: capacitación para el ENARM. Editorial Digital del Tecnológico de Monterrey.
2. Berrios Alvarez, M. D. (2019). Factores asociados a embarazo ectópico en pacientes atendidas en el Hospital Antonio Lorena, Cusco 2018 [Tesis de licenciatura, Universidad Nacional San Antonio de Abad del Cusco]. Repositorio institucional. https://repositorio.unsaac.edu.pe/handle/20.500.12918/4032
3. Bertin, F., Montecinos, M., Torres, P. y Pinto, P. (2019). Embarazo ectópico cornual, diagnóstico y tratamiento: reporte de dos casos y revisión de la literatura. Revista Chilena de Obstetricia y Ginecología, 84(1), 55–63. https://doi.org/10.4067/S0717-75262019000100055.
4. Bombilla Cuayla, S. Y. (2021). Embarazo Ectópico [Trabajo académico de licenciatura, Universidad José Carlos Mariátegui]. Repositorio institucional. https://renati.sunedu.gob.pe/handle/sunedu/3120230
5. Butcher, H. K., Bulechek, G. M., Wagner, C. M., & Dochterman, J. M. (Eds.). (2018). Clasificación de intervenciones de enfermería (NIC). Elsevier.
6. Caballero Muñoz, E., Becerra Salas, R. y Latrach, C. (2005). Utilización del proceso de enfermería. Santiago de Chile: Universidad Mayor.
7. Cabo de Villa, E. D., Morejón Hernández, J. M. y Acosta Figueredo, E. (2020). Dolor y analgésicos. Algunas consideraciones oportunas. MediSur, 18(4), 694-705. https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=99517
8. Cannon, J. W. (2018). Hemorrhagic shock. The New England Journal of Medicine, 378(4), 370–379. https://doi.org/10.1056/nejmra1705649
9. Carpenito, L. J. (2021). Handbook of nursing diagnosis (16ta. Ed.). Jones & Bartlett Learning. Carrillo, R., De La Torre, T., Nava, J. A., Posada, A., Pérez, Á. A., De La Torre, M. A., Cabello, R., & López, M. del R. (2018). Consenso multidisciplinario para el manejo de la hemorragia obstétrica en el perioperatorio. Revista Mexicana de Anestesiología, 41(3), 155–182. https://www.medigraphic.com/pdfs/rma/cma-2018/cma183b.pdf
10. Carvajal Hermida, E. Y., & Sánchez-Herrera, B. (2018). Nursing Care with a Human Approach": A Model for Practice with Service Excellence. Aquichan, 18(2), 149-159. https://aquichan.unisabana.edu.co/index.php/aquichan/article/view/7573
11. Castiblanco, R. A., Coronado, C. M., Morales, L. V., Polo, T. V. y Saavedra, A. J. (2022). Hemorragia postparto: intervenciones y tratamiento del profesional de enfermería para prevenir shock hipovolémico. Revista Cuidarte, 13(1), 1–18. https://doi.org/10.15649/cuidarte.2075
12. Ccayanchira Domínguez, M., & Sicha Cueto, I. S. (2022). Cuidados de enfermería en embarazo ectópico complicado del servicio de Ginecología de un hospital nacional de Ayacucho, 2021 [Trabajo académico de licenciatura, Universidad Peruana Unión]. Repositorio institucional. https://repositorio.upeu.edu.pe/handle/20.500.12840/5739
13. Chiguay Copa, H. A. (2021). Características epidemiológicas, clínicas y quirúrgicas del embarazo ectópico en gestantes atendidas en el Hospital III Goyeneche, Arequipa, en el período enero-diciembre 2020 [Tesis de licenciatura, Universidad San Agustín de Arequipa]. Repositorio institucional. https://repositorio.unsa.edu.pe/items/5f45462e- 3c89-4730-86a5-877430ffa177
14. Chinizaca Torres, D. A. (2019). Prevalencia y factores asociados al embarazo ectópico en mujeres de edad fértil atendidas en el Hospital Vicente Corral Moscoso, periodo 2016-2018 [Trabajo académico de licenciatura, Universidad Católica de Cuenca]. Repositorio institucional. https://dspace.ucacue.edu.ec/items/130872f4-d9e9-44e2-ab83-d04e635affee
15. De la Cruz, S. (2018). Cuidados de enfermería a Pacientes con embarazo ectópico en el servicio de emergencia del Hospital Rezola Cañete 2015 [Trabajo académico de licenciatura, Universidad Nacional del Callao]. Repositorio institucional. http://repositorio.unac.edu.pe/handle/UNAC/2891
16. Fernández Dolón, J. (2022). Historia de la Enfermería. Universidad Pontificia Comillas. Figueredo-Borda, N., Ramírez-Pereira, M., Nurczyk, S., & Diaz-Videla, V. (2019). Modelos Y Teorías De Enfermería: Sustento Para Los Cuidados Paliativos. Enfermería: Cuidados Humanizados, 8 (2). https://doi.org/10.22235/ech.v8i2.1846
17. Garita, S. E., Fernández, J. C. G. y Alvarado, G. P. (2021). Generalidades del embarazo ectópico. Revista Médica Sinergia, 6(5). https://doi.org/10.31434/rms.v6i5.670
18. Gasparri, M. L., Mueller, M. D., Taghavi, K. y Papadia, A. (2018). Conventional versus single port laparoscopy for the surgical treatment of ectopic pregnancy: a meta-analysis. Gynecologic and obstetric investigation, 83 (4), 329-337. https://doi.org/10.1159/000487944
19. Guevara-López, U., Covarrubias-Gómez, A., Delille-Fuentes, R., Hernández-Ortiz, A., Carrillo- Esper, R. y Moyao-García, D. (2005). Parámetros de práctica para el manejo del dolor agudo perioperatorio. Cirugía y Cirujanos, 73(3), 223-232. ttps://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=4406
20. Heather, T. y Kamitsuru, S. (2021). Diagnósticos enfermeros definición y clasificación 2021- 2023. Elsevier.
21. Hendriks E, Rosenberg R. y Prine L. (2020). Ectopic Pregnancy: Diagnosis and Management. American Family Physician, 101 (10), 599-606. https://www.aafp.org/pubs/afp/issues/2020/0515/p599.pdf
22. Herdman, H. y Kamitsuru, S. (2018). NANDA: diagnósticos de enfermería internacionales: definiciones y clasificación (11ma ed.). Elsevier. https://maludice7.com/diagnosticos-de- enfermeria-nanda-i-2018-2020/
23. Huerta Verde, L. V. y López Villanueva, D. J. (2022). Factores de riesgo asociados al embarazo ectópico, hospital Víctor Ramos Guardia Huaraz, 2019 [Tesis de licenciatura, Universidad Nacional Santiago Antúnez de Mayolo]. Repositorio institucional. https://repositorio.unasam.edu.pe/handle/UNASAM/5096
24. Iyer P.E. y Taptich B.J. (2008) Proceso y Diagnóstico de Enfermería (3ra ed.). Editorial Ciencias Médicas. Kislitsina, O. N., Rich, J. D., Wilcox, J. E., Pham, D. T., Churyla, A., Vorovich, E. B., ... y Yancy, C. W. (2019). Shock–classification and pathophysiological principles of therapeutics. Current cardiology reviews, 15(2), 102-113. https://doi.org/10.2174/1573403x15666181212125024
25. Liang, H. H., Vargas, J. S., Sánchez, A. G. H. y Mora, J. V. (2019). Embarazo ectópico: Revisión bibliográfica con enfoque en el manejo médico. Revista clínica de la escuela de medicina de la universidad de Costa Rica, 9(1), 28-36. https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=87031
26. Lizardo Villaorduña, C. M. (2021). Embarazo ectópico complicado en paciente tercigesta en hospital II-2 Huaraz, 2018 [Trabajo académico de licenciatura, Universidad José Carlos Mariátegui]. Repositorio institucional. https://repositorio.ujcm.edu.pe/handle/20.500.12819/1485
27. Mamani Barboza, A. V. (2018). Factores de riesgo asociados al embarazo ectópico de las pacientes atendidas en el Hospital Regional Manuel Nuñez Butron en el periodo de enero a diciembre en el año 2017-Puno [Tesis de bachillerato, Universidad Nacional del Altiplano]. Repositorio institutional. http://repositorio.unap.edu.pe/handle/20.500.14082/8043
28. Marik PE, Weinmann M. (2019). Optimizing fluid therapy in shock. Current Opinion in Critical Care, 25(3), 246-51. https://journals.lww.com/co- criticalcare/abstract/2019/06000/optimizing_fluid_therapy_in_shock.10.aspx
29. Marion, L. L. y Meeks, G. R. (2012). Ectopic pregnancy: history, incidence, epidemiology, and risk factors. Clinical obstetrics and gynecology, 55(2), 376-386. https://journals.lww.com/clinicalobgyn/abstract/2012/06000/ectopic_pregnancyhistory,_incidence,.3.aspx
30. Martínez A, Quintero L, García C. y Fernández, A. (2018). Embarazo ectópico cervical: diagnóstico preciso y enfoque de manejo médico. Reporte de caso. Universitas Médica, 59(1). http://doi.org/10.11144/Javeriana.umed59-1
31. Matos, H., Rodríguez, O., Estrada, G., Martínez, M., Saap, A., Osorio, M., Beltrán, J. y Denis, E. (2018). Caracterización de embarazo ectópico. Revista Información Científica, 97(6), 1100–1110. http://www.revinfcientifica.sld.cu/index.php/ric/article/view/2174/3937
32. Mejía, J. H. (2018). Beneficios del uso de metotrexato vs. del tratamiento quirúrgico en pacientes con embarazo ectópico no complicado en el instituto nacional materno perinatal durante los años 2014-2015 [Tesis de bachillerato, Universidad Ricardo Palma]. https://repositorio.urp.edu.pe/bitstream/handle/20.500.14138/1285/192-JMEJÍA.pdf?sequence=1&isAllowed=y
33. Melgarejo, E. (2018). Proceso de atención de enfermería aplicado a paciente pos operado de laparotomía exploratoria por embarazo ectópico complicado en la Unidad de Recuperación Posanestésica de un hospital de Lima, 2018 [Trabajo académico de licenciatura, Universidad Peruana Unión]. Repositorio institucional. https://repositorio.upeu.edu.pe/handle/20.500.12840/1417
34. Mieles Orlando, A. M. y Rosado Gómez, N. I. (2021). Prevalencia y evaluación del shock hipovolémico por embarazo ectópico en mujeres de 20 a 35 años atendidas en el hospital general norte de Guayaquil, los Ceibos durante el periodo de enero 2017 y 2019 [Tesis de bachillerato, Universidad Católica de Santiago de Guayaquil]. Repositorio institucional. http://repositorio.ucsg.edu.ec/handle/3317/16762
35. Moltó, B. (2022). Proceso de atención de enfermería en un paciente con embarazo ectópico ovárico. Caso clínico. Revista Electrónica de Portales Médicos, 17(7), 279. https://www.revista-portalesmedicos.com/revista-medica/proceso-de-atencion-de- enfermeria-en-un-paciente-con-embarazo-ectopico-ovarico-caso-clinico/
36. Moorhead, S., Swanson, E., Johnson, M. y Maas, M. L. (2018). Clasificación de resultados de enfermería (NOC): medición de resultados en salud (6ta ed.). Elsevier.
37. Morales Baldeón, M. (2018). Manejo de las complicaciones en el embarazo ectópico [Trabajo académico de titulación, Universidad de Guayaquil. Repositorio institucional. https://repositorio.ug.edu.ec/items/1177f726-74be-4808-af54-4775e21f6587
38. Murillo, M. (2020). Abordaje enfermero del embarazo ectópico [Trabajo académico de fin de grado, Universidad Católica de Murcia]. Repositorio institucional. https://repositorio.ucam.edu/handle/10952/4953
39. Naranjo-Hernández, Y., González-Hernández, L. y Sánchez-Carmenate, M. (2018). Proceso Atención de Enfermería desde la perspectiva docente. Revista Archivo Médico de Camagüey, 22(6), 831-842. http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1025-02552018000600831&lng=es&tlng=es.
40. Núñez, E. y Panta, O. (2018). Enfermedad pélvica inflamatoria, embarazo ectópico previo y anteceden-te de cirugía tubárica como factores de riesgo de embarazo ectópico. Servicio de Ginecología del Hospital Regional Docente de Trujillo, 2000-2015. Revista Ciencia y Tecnología, 14(3), 89-95. https://revistas.unitru.edu.pe/index.php/PGM/article/view/2109
41. Pacagnella, R. C. y Borovac-Pinheiro, A. (2019). Assessing and managing hypovolemic shock in puerperal women. Best Practice & Research Clinical Obstetrics & Gynaecology, 61, 89- 105. https://doi.org/10.1016/j.bpobgyn.2019.05.012
42. Palomar-Aumatell, X. (2017). 2. Uso De Un Indicador NOC para valorar la Cinetosis. Universitat Central de Catalunya. http://hdl.handle.net/10854/4969 Parra, A. I. R. (2019). Embarazo ectópico. Revista Médica Nasajpg, 1.
43. Pérez Pacheco, F. S. (2022). Proceso de atención de enfermería a paciente con embarazo ectópico y abdomen agudo, del servicio de emergencia de ginecobstetricia de un hospital de Lima, 2021 [Trabajo académico de licenciatura, Universidad Peruana Unión. Repositorio institucional. https://repositorio.upeu.edu.pe/handle/20.500.12840/5367
44. Pesut, D. J. y Herdman, J. (2019). Razonamiento clínico: el arte y la ciencia del pensamiento crítico y creativo. Elsevier.
45. Pincay González, E. A. (2021). Aplicación del proceso enfermero en usuaria con embarazo ectópico tubárico. Hospital Básico Rafael Serrano López La Libertad 2020 [Trabajo académico de licenciatura, Universidad Estatal Península de Santa Elena]. Repositorio institucional. https://repositorio.upse.edu.ec/handle/46000/5764
46. Quispe, R. (2019). Prevalencia y factores de riesgo asociados a embarazo ectópico en el área de ginecología y obstetricia del Hospital Regional de Ayacucho periodo septiembre 2017 - septiembre 2018 [Tesis de bachillerato, Universidad Nacional del Altiplano]. Repositorio institucional. http://repositorio.unap.edu.pe/handle/20.500.14082/11076
47. Ramos, A., Guajardo, J., Chejne, F., Juárez, Á. y Ayón, H. (2018). Mecanismos para prevenir dolor agudo a crónico. Revista Mexicana de Anestesiología, 41(1), 44–47. http://www.medigraphic.com/rmawww.medigraphic.org.mx
48. Riegel, F., Oliveira, M. da G. y Silveira, D. (2018). Contribuições da teoria de Jean Watson ao pensamento crítico holístico do enfermeiro. Revista Brasileira de Enfermagem, 71(4), 2193–2197. http://www.scielo.br/pdf/reben/v71n4/pt_0034-7167-reben-71-04-2072.pdf
49. Román-Soto, J., Oyola-García, A. y Quispe-Ilanzo, M. (2019). Factores de riesgo de hemorragia primaria posparto. Revista Cubana de Medicina General Integral, 35(1), 1–12.
50. Ruiz Fernández, M. D. C., Siles Carvajal, A., & Silva Muñoz, G. (2019). Gestación ectópica. Una consulta de urgencias en el primer trimestre. Diagnóstico y tratamiento. Recuperado de: http://ciberfebrero2019.enfermeriadeurgencias.com/images/4.pdf
51. Ruiz Freire, B. Y. (2022). Proceso de atención de enfermería en gestante de 28 años con embarazo ectópico de 6 semanas de gestación [Examen complexivo de enfermería, Universidad de Babahoyo]. Repositorio institucional. http://dspace.utb.edu.ec/handle/49000/11461
52. Sánchez Rodríguez, J. R., Aguayo Cuevas, C. P. y Galdames Cabrera, L. (2017). Desarrollo del conocimiento de enfermería, en busca del cuidado profesional. Relación con la teoría crítica. Revista Cubana de Enfermería, 33 (3). https://revenfermeria.sld.cu/index.php/enf/article/view/2091
53. Tian, N., Yu, J., Zhang, S., Ma, W., Wang, T. y Wang, Y. (2018). Effects of methotrexate on the quality of oocyte maturation in vitro. European Biophysics Journal, 47, 249-260. https://link.springer.com/article/10.1007/s00249-017-1254-2
54. Torcal Baz, M. y Ventoso Mora, S. A. (2020). Manejo y tratamiento del dolor en cuidados paliativos. Revista Clínica de Medicina de Familia, 13(3), 203-211. https://revclinmedfam.com/article/manejo-y-tratamiento-del-dolor-en-cuidados-paliativos
55. Vernaza, P., Posadas, L. & Acosta, C. (2019). Dolor y emoción, una reflexión para el profesional en ciencias de la salud. Duazary, 16(1), 145 - 155. https://doi.org/10.21676/2389783X.2639
FINANCING
The authors received no funding for the development of this research.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Olivia E. Pulcha-Llerena, Sofía D. Vivanco-Hilario, Wilter C. Morales-García.
Drafting - original draft: Olivia E. Pulcha-Llerena, Sofía D. Vivanco-Hilario, Wilter C. Morales-García.
Writing - proofreading and editing: Olivia E. Pulcha-Llerena, Sofía D. Vivanco-Hilario, Wilter C. Morales-García.