doi: 10.62486/agmu202494
CASE REPORT
Bladder Lymphoma. Presentation of clinical case
Linfoma de vejiga. Presentación de caso clínico
Lucien G.
Bory Porras1 ![]() *, Jadier Wong Silva2
*, Jadier Wong Silva2 ![]() , Yarilis Fabregas Valle1
, Yarilis Fabregas Valle1 ![]() , Deisy Martínez García1
, Deisy Martínez García1 ![]() , Maidelys Ortega Rodríguez1
, Maidelys Ortega Rodríguez1 ![]() , Roberto Ortiz Benet3
, Roberto Ortiz Benet3 ![]()
1Universidad de Ciencias Médicas de Pinar del Río. Hospital General “Abel Santamaría Cuadrado”. Pinar del Río, Cuba.
2Hospital Pediátrico Provincial Docente “Pepe Portilla”. Universidad de Ciencias Médicas de Pinar del Río. Cuba.
3Instituto Nacional de Oncología y Radiobiología. La Habana. Cuba.
Cite as: Bory Porras LG, Wong Silva J, Fabregas Valle Y, Martínez García D, Ortega Rodríguez M, Ortiz Benet R. Bladder Lymphoma. Presentation of clinical case. Multidisciplinar (Montevideo). 2024; 2:94. https://doi.org/10.62486/agmu202494
Submitted: 08-12-2023 Revised: 18-03-2024 Accepted: 07-08-2024 Published: 08-08-2024
Editor: Telmo
Raúl Aveiro-Róbalo ![]()
ABSTRACT
Introduction: lymphomas develop in lymphoid tissue located in lymph nodes and in dissimilar organs of the human body. They are malignant tumors located in the lymphoid tissue with a low incidence in the genitourinary tract as the primary site; among them, those of the bladder are uncommon. Primary bladder lymphomas present an indistinguishable clinical-radiological pattern, of solid growth and with characteristics similar to urothelial carcinoma.
Objective: to present a clinical case, with a diagnosis of primary bladder lymphoma treated in the Oncology service of the “Abel Santamaría Cuadrado” General Teaching Hospital in Pinar del Río.
Case presentation: patient, 58 years old, male, white, relative health history; In February 2020, he went to the clinic due to bleeding in his urine, urinary urgency, droplet urination, as well as weight loss of more than 15 lbs. and evening fever. He was evaluated by the urology service, which suspected urothelial carcinoma of the bladder, which led to a systematic diagnosis that determined infiltration of the bladder wall by intermediate B cell non-Hodgkin lymphoma.
Conclusions: the diagnosis in these cases is determined by immunohistochemistry studies and tumor monoclonality demonstrated by molecular biology techniques. Primary bladder lymphomas have a solid growth pattern similar to that of urothelial carcinoma. The choice for treatment consists of a regimen consisting of CHOP chemotherapy (cyclophosphamide, vincristine, prednisone, doxorubicin) combined with the anti-CD20 monoclonal antibody rituximab. We present a case of infradiaphragmatic intermediate B cell non-Hodgkin lymphoma with extralymphatic involvement of the bladder.
Keywords: Primary bladder lymphoma; Immunohistochemistry; Chemotherapy.
RESUMEN
Introducción: los linfomas se desarrollan en el tejido linfoideo localizado en ganglios linfáticos y en los disímiles órganos del cuerpo humano. Son tumores malignos localizados en el tejido linfoideo con baja incidencia en el tracto genitourinario como sitio primario, dentro de ellos, los de vejiga son infrecuentes. Los linfomas primarios de vejiga presentan un patrón clínico-radiológico indistinguible, de crecimiento sólido y con características similares al carcinoma urotelial.
Objetivo: presentar un caso clínico, con diagnóstico de linfoma primario de vejiga tratado en el servicio de Oncología del Hospital General Docente “Abel Santamaría Cuadrado” de Pinar del Río.
Presentación de caso: paciente de 58 años de edad, sexo masculino, raza blanca, antecedentes de salud relativa; en febrero de 2020 acude a consulta por mostrar sangrado en la orina, tenesmo vesical, micción en gotas, además de pérdida de peso de más de 15 lb y fiebre vespertina. Fue valorado por el servicio de urología que sospechó un carcinoma urotelial de vejiga lo que conllevó una sistemática diagnóstica que determinó una infiltración a pared vesical de Linfoma no Hodgkin de células intermedias B.
Conclusiones: el diagnóstico en estos casos es determinado por los estudios de Inmunohistoquímica y la monoclonalidad tumoral demostrada por las técnicas de biología molecular. Los linfomas primarios de vejiga poseen un crecimiento sólido patrón similar al del carcinoma urotelial. La elección para el tratamiento consiste en un esquema conformado por quimioterapia CHOP (ciclofosfamida, vincristina, prednisona, doxorrubicina) unido al anticuerpo monoclonal anti-CD20 rituximab. Se presenta un caso de linfoma no Hodgkin de células intermedias B infradiafragmático con compromiso extralinfático de vejiga.
Palabras clave: Linfoma Primario de Vejiga; Inmunohistoquímica; Quimioterapia.
INTRODUCTION
Eve and Chaffey first described primary bladder lymphomas in 1885; since then, around 100 cases have been published.(1,2) Large B-cell and marginal zone lymphomas are the most common types. Extranodal lymphomas account for 0,2 % of all lymphomas, demonstrating that they are scarce.(3) There is a higher incidence in women, with a frequency of occurrence 6,5 times higher than in men. The average age of onset is 64 years, with a range of 20 to 85 years. The etiology in these cases is not yet well defined.
The location presented by the patient in this study is exceptional. The data from most published and consulted studies on large cell non-Hodgkin lymphomas show an extra ganglionic location but a low presence in this organ.(4) The clinical and radiographic symptoms are similar to those of urothelial carcinoma, and molecular and immunohistochemical studies are required for diagnosis. Taking this entity into account, urine cytology can sometimes diagnose the tumor.(5)
Although, in the present case, the absence of t (14:18) translocation and the negative result with the bcl-2 immunohistochemical antibody rule out the possibility of the lymphoma originating in the follicular center cells, it may still be present. In the bladder, a close relationship between chronic bacterial infections and lymphomas has been studied, with greater emphasis on cases of MALT lymphomas.(6)
CASE PRESENTATION
A 58-year-old white male patient with no previous medical history reported during the medical interview that approximately 7 months ago, he began experiencing urinary symptoms characterized by blood in the urine, bladder tenesmus, dribbling urination, as well as weight loss of more than 15 lb, and afternoon fever. The Urology Service evaluated him at the Abel Santamaría Cuadrado General Teaching Hospital, and a cystoscopy was performed.
Physical examination: In the hypogastrium, there is a 5 cm open surgical scar with no associated sepsis; the rest is unremarkable. (See the following figure 1).

Figure 1. Surgical scar, 5 cm open and without associated sepsis
Rectal examination: Prostate enlarged (grade II), flat adenomatous.
Additional findings:
· HB 14,6 g/l
· Platelet count 360 x 109/L
· Lts 8,3 x 109/L, lymphocytes 32 %, PMN 60 %
· Erythrocytes: 5 mm/h
· Blood glucose: 5,7 mmol/L
· GPT: 15 U/I
· TGO: 30 U/I
· Alkaline phosphatase: 139 U/I.
· Total protein: 72 g/l
· Total bilirubin: 6
· Indirect bilirubin: 4
· Direct bilirubin: 2,5
· Creatinine: 92 mmol/l
· LDH: 138 mmol/l
· HCV, HBV, HIV, VDRL: Negative
· Urinary cytology: Cytological smear from urinary cytology, 4 slides examined with low cell count, identifying epithelial cells without atypia, some polymorphonuclear neutrophils, and debris in the background.
Imaging studies
· Echocardiogram: No abnormalities, LVEF: 73 %
· Abdominal ultrasound: Marked increase in liver echogenicity with distortion of its architecture, IR two cystic images greater than 38 mm on the anterior surface, inside the bladder there is a low echogenic mass 38 cm in diameter with well-defined contours; cystoscopy is recommended.
· AP chest X-ray: No pleuropulmonary changes described.
· Contrast-enhanced computed axial tomography: Neck, thorax, abdomen, and pelvic bones: Partial thickening of both vocal cords and partial thinning of the piriform sinus, small bilateral axillary adenopathies, no bilateral mediastinal adenopathies, irregularity of the bronchial walls, with good permeability of the main bronchi, slight degenerative changes in the cervical-dorsal region, more pronounced in the lower dorsal segment. No pulmonary nodules or pleural effusion.
· Abdomen: No focal liver lesions, spleen with slight splenomegaly at a depth of 74 mm, pancreas and both kidneys normal, small cysts measuring 4 mm, marked thickening of the subcutaneous tissue 4 cm below the umbilical region, with thickening of the muscles at the midline and in close contact with the bladder wall, which is evidenced by ultrasound as a 4,2 cm bladder tumor, which is retracted, with obliteration of the perivesical fat, small perivesical and deep inguinal adenopathies adjacent to the seminal vesicles, no retroperitoneal lymph nodes, moderate degenerative changes in the lumbosacral spine, osteosclerotic image at the level of the middle sacral wall, as well as the left iliac hip measuring 7 mm and the right iliac hip measuring 10 mm.
· Cystoscopy: Panendoscopy performed, observing increased volume of both prostate lobes occluding the urethral lumen, at the level of the prostatic urethra, reliable tissue, bladder tumor infiltrating the right lateral wall, where transurethral resection performed and biopsy taken.
Anatomical pathological studies
· Bone marrow examination: Bone marrow not infiltrated by tumor.
· Bone marrow biopsy: Bone marrow not infiltrated by lymphoma.
· Pathological biopsy: Multiple tissue fragments consisting of grade IV urothelial carcinoma with lymphatic tumor invasion, non-blood, and acute chronic inflammatory reaction are examined.
Pathological Anatomy at the “Hermanos Ameijeiras Hospital”
· Infiltration of the bladder wall by non-Hodgkin lymphoma of intermediate B cells.
· Immunohistochemistry (IHC):
· PAX5: positive
· CD79a: positive
· CD43: negative
· LCA: positive
· BCL6: positive
· CD43: negative
· KI67: 50 %
Treatment received
He received 14 x 6 cycles of CHOP chemotherapy and consolidation radiotherapy on the affected site. A complete clinical response was achieved and the patient remained under oncological follow-up.
Figure 2. Surgical scar after 6 cycles of CHOP 14
PET/CT response evaluation studies: The PET study and PET-CT fusion images did not reveal any abnormal areas of glycolytic hypermetabolism.
Physiological biodistribution of the tracer in the rest of the body.
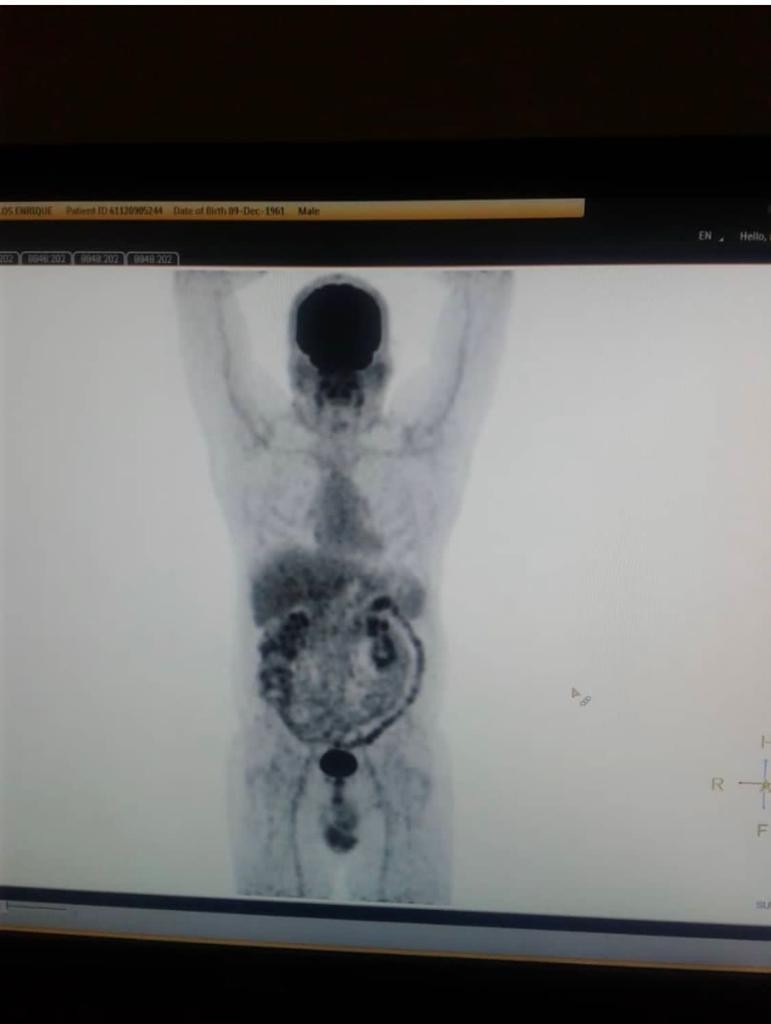
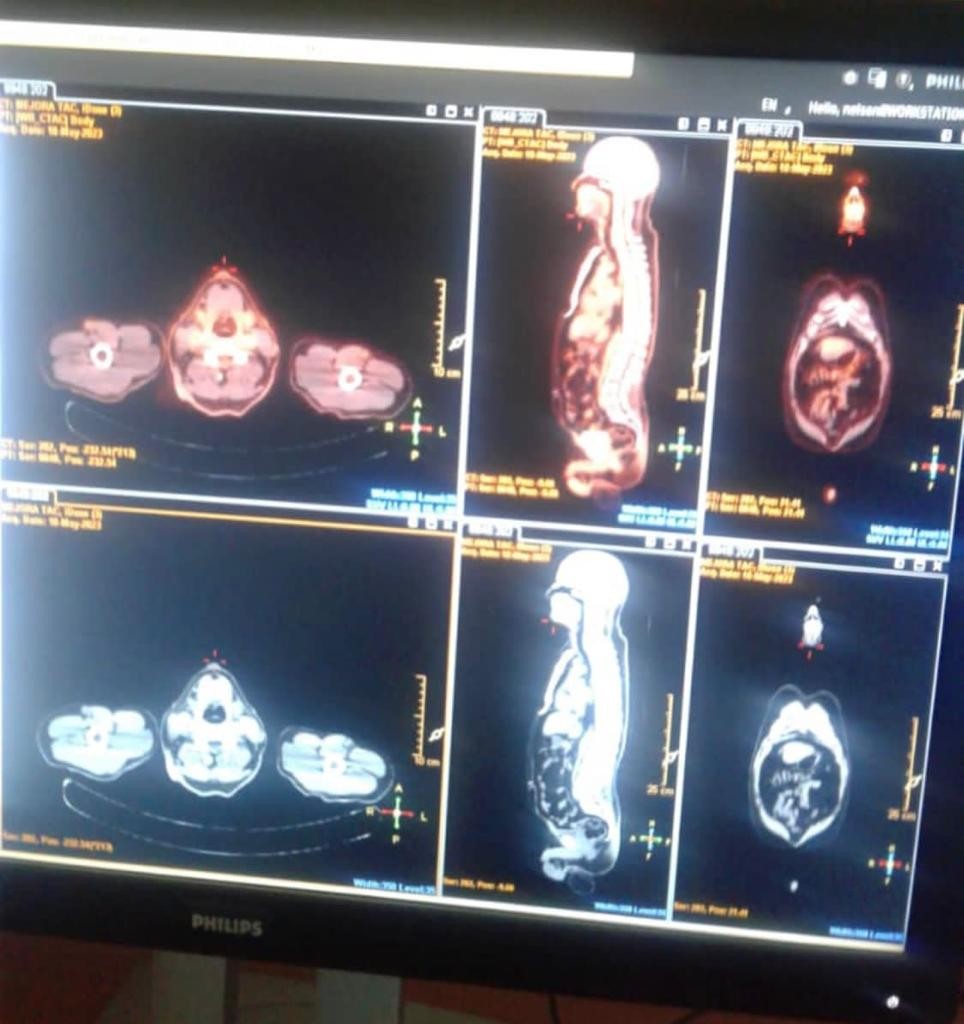
Figure 3. PET/CT images
DISCUSSION
Bladder lymphomas are more common in women over the age of 60, usually white, with a ratio of 3:1 compared to men. Chronic cystitis is associated with 50 % of cases.(6)
There are three types of presentation: primary form occurs in 17 % of cases, systemic diseases present in 47 %, and secondary form occurs in 36 %. Diffuse large cell lymphoma occurs most frequently as a secondary form, followed by follicular lymphomas, low-grade MALT, Burkitt, Hodgkin, and mantle cell lymphomas. Bladder tumors account for less than 0,5 % of bladder tumors.(6)
The clinical manifestations and radiological characteristics are indistinguishable from those of urothelial bladder tumors. Immunohistochemical techniques, histopathological samples, and molecular biology are vital for diagnosis.(7) They usually present as gross hematuria of varying intensity, with dysuria and pollakiuria in 77 % of cases. In primary bladder lymphomas, obstructive uropathy is uncommon, as it does not affect the ureteral orifices.(8) This presentation is more common (17,2 %) in secondary bladder lymphomas, occurs in advanced stages of the disease, and is caused by adenopathies in the lower pelvis or extrinsic compression of the urinary tract at the trigone.(9)
Macroscopically, solid submucosal masses, which are multinodular and ulcerated in a few cases, are observed. Histology is generally diffuse, with long cells and small lymphocytes, with immunohistochemistry compatible with B-cell lineage.(6)
Surgical treatment is justified to obtain greater certainty in the histological diagnosis after transurethral resection. The tumor is sensitive to radiation and chemotherapy, so external radiation therapy is indicated for localized tumors and confined organs in conjunction with non-aggressive surgery or alone. It should be noted that clinical remission is only possible with polychemotherapy treatment.(10) CHOP chemotherapy (vincristine, doxorubicin, cyclophosphamide, and prednisone) and anti-CD20 antibodies are used.(9) The prognosis is generally favorable when the tumor is confined to one organ. The 5-year survival rate is 50 %.(7,9)
CONCLUSIONS
Primary bladder lymphoma is rare and is indistinguishable from other bladder tumors. It generally responds well to chemotherapy. The prognosis is good for disseminated forms of the disease. In our case, the patient received six cycles of CHOP chemotherapy and RTP at the affected site, with a good response to treatment, 30 months of progression-free survival, and an overall survival of 44 months.
REFERENCES
1. Khaitan A, Gupta NP, Goel A, Safaya R, Kumar L. Primary non-Hodgkin´s lymphoma of urinary bladder. Report of a case and review of the literature. Urol Int [Internet] 2018 [citado 12/11/2023]; 72:82-84. Disponible en: https://pubmed.ncbi.nlm.nih.gov/14730173/
2. Bates AW, Norton AJ, Baithun SI Malignant lymphoma of the urinary bladder: a clinicopathological study of 11 cases. J Clin Pathol [Internet] 2000 [citado 12/11/2023]; 53:458-461. Disponible en: https://pubmed.ncbi.nlm.nih.gov/10911804/
3. Al-Maghrabi J, Kamel-Reid S, Jewett M, Gospodarowicz M, Wells W, Banerjee D. Primary low-grade cell-B lymphoma of mucosa-associated lymphoid tissue type arising in the urinary bladder: report of 4 cases with molecular genetic analysis. Arch Pathol Lab Med [Internet] 2021 [citado 12/11/2023]; 125 (3):332-336. Disponible en: https://pubmed.ncbi.nlm.nih.gov/11231478/
4. Eble J, Sauter G, Epstein JI, Sesterhenn IA. World Health Organization Classification of Tumours. Pathology and genetics of tumours of the urinary system and male genital organs. 1st ed. Lyon: IARC press, 2019.
5. Jaudah Al-Maghrabi, MD, Suzanne Kamel-Reid PhD, Michael Jewett MD, et al. Primary low-grade B-Cell lymphoma of mucosa-associated lymphoid tissue type arising in the urinary bladder. Archives of Pathology and Laboratory Medicine. [Internet] 2021 [citado 12/11/2023]; 125: 332–336. Disponible en: https://pubmed.ncbi.nlm.nih.gov/11231478/
6. Álvarez Álvarez C, Vieites Pérez-Quintela B, Pesqueira Santiago D, et al. Linfoma no Hodgkin B de célula grande primario de vejiga. Actas Urol Esp [Internet] 2015 [citado 12/11/2023]; 29 (9): 902-904. Disponible en: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0210-48062005000900014
7. Sharma A, Singh AB. Primary lymphoma of urinary bladder: report of an unusual case and literature review. The Internet Journal of Urology. [Internet] 2022 [citado 12/11/2023]; 1: 1. Disponible en: https://ispub.com/IJU/1/1/3602
8. García Ligero J, Navas Pastor J, García García A, et al. Tumor transicional intraureterocele sincrónico a tumor ureteral contralateral: uropatía obstructiva en enfermedad panurotelial. Arch. Esp. Urol. [Internet] 2002 [citado 12/11/2023]; 55, 4:443-446. Disponible en: https://pesquisa.bvsalud.org/portal/resource/pt/ibc-13237
9. Martín Laborda y Bergasa F, Lozano Lozano D, Gil Fernández JJ, et al. Linfoma no Hodgkin y aparato urinario. A propósito de un caso. Actas Urol Esp. [Internet] 2015 [citado 12/11/2023]; 29 (4): 427-432. Disponible en: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0210-48062005000400017
10. Manoj Monga MD, Lamia L, Gabal-Shehab MD, et al. Primary lymphoma of the bladder. Infect Urol. [Internet] 2020 [citado 12/11/2023]; 13(3):82-84. Disponible en: https://www.elsevier.es/es-revista-cirugia-espanola-36-pdf-S021048060573268X
FUNDING
The authors did not receive funding for the development of this research.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
CONTRIBUTION OF AUTHORS
Conceptualization: Lucien G. Bory Porras, Jadier Wong Silva, Yarilis Fabregas Valle, Deisy Martínez García, Maidelys Ortega Rodríguez, Roberto Ortiz Benet.
Data curation: Lucien G. Bory Porras, Jadier Wong Silva, Yarilis Fabregas Valle, Deisy Martínez García, Maidelys Ortega Rodríguez, Roberto Ortiz Benet.
Formal analysis: Lucien G. Bory Porras, Jadier Wong Silva, Yarilis Fabregas Valle, Deisy Martínez García, Maidelys Ortega Rodríguez, Roberto Ortiz Benet.
Research: Lucien G. Bory Porras, Jadier Wong Silva, Yarilis Fabregas Valle, Deisy Martínez García, Maidelys Ortega Rodríguez, Roberto Ortiz Benet.
Methodology: Lucien G. Bory Porras, Jadier Wong Silva, Yarilis Fabregas Valle, Deisy Martínez García, Maidelys Ortega Rodríguez, Roberto Ortiz Benet.
Project management: Lucien G. Bory Porras, Jadier Wong Silva, Yarilis Fabregas Valle, Deisy Martínez García, Maidelys Ortega Rodríguez, Roberto Ortiz Benet.
Resources: Lucien G. Bory Porras, Jadier Wong Silva, Yarilis Fabregas Valle, Deisy Martínez García, Maidelys Ortega Rodríguez, Roberto Ortiz Benet.
Software: Lucien G. Bory Porras, Jadier Wong Silva, Yarilis Fabregas Valle, Deisy Martínez García, Maidelys Ortega Rodríguez, Roberto Ortiz Benet.
Supervision: Lucien G. Bory Porras, Jadier Wong Silva, Yarilis Fabregas Valle, Deisy Martínez García, Maidelys Ortega Rodríguez, Roberto Ortiz Benet.
Validation: Lucien G. Bory Porras, Jadier Wong Silva, Yarilis Fabregas Valle, Deisy Martínez García, Maidelys Ortega Rodríguez, Roberto Ortiz Benet.
Visualization: Lucien G. Bory Porras, Jadier Wong Silva, Yarilis Fabregas Valle, Deisy Martínez García, Maidelys Ortega Rodríguez, Roberto Ortiz Benet.
Writing – original draft: Lucien G. Bory Porras, Jadier Wong Silva, Yarilis Fabregas Valle, Deisy Martínez García, Maidelys Ortega Rodríguez, Roberto Ortiz Benet.
Writing – review and editing: Lucien G. Bory Porras, Jadier Wong Silva, Yarilis Fabregas Valle, Deisy Martínez García, Maidelys Ortega Rodríguez, Roberto Ortiz Benet.