doi: 10.62486/agmu202498
ORIGINAL
Nursing role in the care
of a patient with threatened abortion in the obstetrics and gynecology service
of a hospital
Rol de enfermería en el
cuidado a paciente con amenaza de aborto del servicio de ginecoobstetricia de
un hospital
Marcela F. Monzón-Murillo1,
Sofía D. Vivanco-Hilario1, Wilter C. Morales-García1  *
*
1Unidad
de Posgrado de Ciencias de la Salud, Universidad Peruana Unión, Escuela de
Posgrado. Lima, Perú.
Cite as:
Monzón-Murillo MF, Vivanco-Hilario SD, Morales-García WC. Nursing
role in the care of a patient with threatened abortion in the obstetrics and
gynecology service of a hospital. Multidisciplinar (Montevideo). 2024; 2:98. https://doi.org/10.62486/agmu202498
Submitted: 20-12-2023
Revised: 04-04-2024 Accepted: 08-08-2024
Published: 09-08-2024
Editor: Telmo
Raúl Aveiro-Róbalo 
ABSTRACT
The threat of abortion is an
alert with vaginal bleeding in the first twenty weeks, accompanied by physical
and emotional suffering. The common complication is mild to severe anemia.
There are no preventive measures to avoid it, so prenatal control is important
so that the pregnancy is viable. In order to know the role of nursing in the
care of patients with threatened abortion, a qualitative study was carried out,
with a single clinical case design based on the Nursing Care Process method,
applying as an instrument the evaluation guide of Marjory Gordon to a
22-year-old patient. 10 nursing diagnoses were identified, prioritizing the
diagnosis: (00221) Ineffective maternity process r/c with insufficient prenatal
care and inadequate maternal nutrition m/p inadequate prenatal management,
ineffective management of bothersome symptoms during pregnancy and prenatal
lifestyle inappropriate. The interventions carried out were satisfactory, since
the patient improved the maternity process. Given the problem of hemorrhage
complication, the results are still indefinite due to the few hours of
intervention and evaluation. It is concluded that the role of nursing is
essential in the assessment of pregnant women with threatened abortion; Knowing
its evolution allowed administering care to resolve the process of ineffective
motherhood and prioritizing individualized nursing care in the prevention of
hemorrhage in the first 20 weeks of pregnancy. In addition, in order to improve
the skills of the nursing professional, NANDA I, NOC, NIC, and collaboration
problems were used.
Keywords: Nursing Role; Care; Patient; Threatened Abortion.
RESUMEN
La amenaza
de aborto, es una alerta con sangrado vaginal en las primeras veinte semanas,
acompañada de sufrimiento físico y emocional. La complicación común es la
anemia de leve a severa. No existen medidas preventivas para evitarlo, por lo
que es importante el control prenatal a fin que el embarazo sea viable. Con el objetivo
de conocer el rol de enfermería en la atención de paciente con amenaza de
aborto, se realizó un estudio cualitativo, con diseño de caso clínico único
basado en el método del Proceso de Atención de Enfermería, aplicando como
instrumento la guía de valoración de Marjory Gordon a una paciente de 22 años.
Se identificaron 10 diagnósticos de enfermería, priorizando el diagnóstico:
(00221) Proceso de maternidad ineficaz r/c con cuidados prenatal insuficiente y
nutrición materna inadecuada m/p manejo prenatal inadecuado, manejo ineficaz de
los síntomas molestos durante el embarazo y estilo de vida prenatal inadecuado.
Las intervenciones ejecutadas fueron satisfactorias, pues la paciente mejoró el
proceso de maternidad. Ante el problema de complicación de hemorragia los
resultados aún son indefinidos debido a las pocas horas de intervención y
evaluación. Se concluye que el rol de enfermería es fundamental en la
valoración de la gestante con amenaza de aborto; conocer su evolución permitió
administrar cuidados para resolver el proceso de maternidad ineficaz y
priorizar los cuidados de enfermería individualizado en la prevención de
hemorragia en las primeras 20 semanas de embarazo. Además, a fin de mejorar las
competencias del profesional de enfermería, se hizo uso del NANDA I, NOC, NIC,
y de los problemas de colaboración.
Palabras clave: Rol
de Enfermería; Cuidado; Paciente; Amenaza de Aborto.
INTRODUCTION
Threatened abortion, as a global
problem, implies a condition with early pregnancy loss or the possibility of
miscarriage before 20 weeks of gestation, characterized by pain and/or
bleeding, closed cervix, evidence of fetal heartbeat by ultrasound, and
intrauterine gestation commensurate with gestational age (Carvajal-Cabrera
& Barriga- Cosmelli, 2021).
According to the World Health
Organization (WHO), between 4,7 % and 13,2 % of annual maternal mortality is
attributed to unsafe abortions; during the years 2010 to 2014, 39 induced
abortions occurred per 1000 women between 15 and 49 years of age (WHO, 2017).
On the other hand, between the years 2015 and 2019, there was an annual average
of 73,3 million unsafe or unsafe induced abortions worldwide. In developing
countries, each year, about 7 million women are hospitalized for unsafe
abortion. In addition, an estimated 121 million unintended pregnancies occurred
each year between 2015 and 2019; and between 4,7 % and 13,2 % of maternal
mortality can be attributed to unsafe abortion each year (WHO, 2020). Of
unintended pregnancies, 61 % ended in abortion, which translates to 73 million
abortions per year worldwide (Frederico et al., 2020).
At the Latin American country level,
only 1 in 4 abortions were safe, while most of them were considered "less
safe". They estimate that 3,7 million induced abortions occur each year in
Latin America and the Caribbean, and they estimate that 17 % of maternal deaths
are due to unsafe abortion.(WHO, 2017) In South America, 10 deaths due to
unsafe abortion occur for every 10 000 live births (WHO, 2020). In this sense,
Ramos (2016) states that it is essential to disseminate and understand the
situation of abortion, as well as the causes, consequences, and difficulties.
The main issues that women face in
deciding to terminate their pregnancies, as well as the attitudes of the
various social actors in favor or against the decriminalization of abortion,
and the respective actions that are practiced in private and public
institutions.
While Ramos and Fernández Vázquez (2020)
note that in the 1990s, maternal mortality was 100 times higher than in
developed countries, this mainly affected poor women, making them more
vulnerable. Likewise, Huanca-Morales (2020) points out that maternal mortality
rates are a sign of women's low capacity for negotiation and self-determination.
In Peru, maternal mortality from unsafe
abortion is the fourth leading cause (Rivero Navia & Pintado Abad, 2017).
In 2015, there were 414 maternal deaths reported by the Peruvian General
Directorate of Epidemiology, but it is not detailed how many of these were
caused by clandestine abortions (Abanto-Arana & Anhuamán-Morillo, 2019).
For its part, INEI (2019) reports 57,8
deaths caused by abortion corresponding to 578 130 live births. In this
country, therapeutic abortion has been legal since 1924; however, exact figures
are not available, although the impact of unsafe abortion is recorded, which
causes 28 652 hospitalizations and 58 deaths each year. In addition, failure to
decriminalize abortion results in 27 166 hospitalizations and 54 deaths per year
in Peru.
It should be noted that the threat of
miscarriage in the first twenty weeks of gestation, if not controlled in time,
leads to the risk of spontaneous termination of pregnancy with bleeding from
the uterus and no changes in the cervix (Dulay, 2020); therefore, the present
research attempts to identify the present problems and/or needs of the patient
through a thorough assessment to issue nursing diagnoses, keeping interest in
the primary diagnosis, as well as the
prevention of the risks of complications
that could be generated in the patient; given that the vaginal bleeding that
could occur as a consequence of an uncontrolled active abortion could generate
secondary hypovolemic shock exceeding blood volume losses of more than 40 %.
In this sense, the obstetrics and
gynecology nursing professional must provide competent human care, promote
timely care, and prevent complications through techniques and procedures that
avoid events that could cause maternal death (Diaz Rivera, 2017).
Therefore, and in light of the scenario
above, the present study aims to confirm the contribution of nursing in the
timely identification of the risk factors that cause miscarriage and prevent
it. Abortion can be defined as the termination of pregnancy before 20 weeks of
gestation, caused by different factors, including genetic, pathological, and
induced factors. In this context, the risks are increased in women who have had
miscarriages, exposure to toxins, placental, cervical, or uterine problems,
among others (Bergallo et al., 2018).
In addition, this work consists of a
qualitative study of a case chosen to analyze, from a
bio-psycho-socio-spiritual point of view, the importance of the nursing
approach in patients with threatened abortion, considering that nursing is the
first contact that patients have after receiving the medical diagnosis, in
addition to sharing difficult and intimate situations with them
(Martínez-Montaño, 2021).
Objectives
Overall
objective
To know the role of nursing in the care
of a patient with threatened abortion.
Specific Objectives
To study the threat of miscarriage, its
risk factors, treatment, and complications. Describe the importance of nursing
care in the prevention of hemorrhage.
Write nursing care in the care of the
effective maternity process for a patient with a threatened abortion.
Develop a nursing care plan based on a
patient with threatened miscarriage using NANDA taxonomy I, NOC, NIC, and Linda
Juall Carpenito's collaborative problem manual (Johnson et al., 2007;
"NANDA Nursing Diagnoses: Definitions and Classification 2018-2020,"
2019).
Theoretical
framework
Abortion
According to Bergallo et al. (2018)
abortion comprises the expulsion, through the uterus, of the product of
conception, causing the termination of pregnancy abruptly, in a natural or
voluntary way, before 22 weeks of gestation, with a fetus weighing less than
500 grams.
Epidemiology of abortion
According to León et al. (2016), 52 % of
women in Peru have abortions because "they have many children" or
"they did not have a stable partner". Twenty-eight percent reveal
that they did so for economic reasons, 8 % for fear of their parents, and 5 %
for having suffered rape or incest. These reasons are similar to those in other Latin American countries.
Risk Factors
There is evidence of a high frequency of
miscarriage incidence in the following cases: when the patient has anatomical
uterine anomalies; when the correction of the uterine anomaly is not possible;
when the patient has an anomalous uterine anomaly.
The surgical procedure has decreased the
incidence of first trimester losses, mainly in recurrent abortion; with the
presence of polyps of more than 2 cm, greater number and size of uterine
fibroids that hinder implantation and deficient blood supply to the fetus; when
rapidly growing and degenerating tumors appear with cytokine release; when
submucosal location or total occupation of the uterine space appears that
hinders the growth of the fetus and uterine adhesions, although at this point
more evidence is needed (Gaspar-Huánuco & Torres-Rojas, 2018).
Types of abortion
WHO (2019) recognizes 4 types of
abortion according to causes and conditions:
Spontaneous abortion
It consists of the termination of a
pregnancy that is not intentionally induced, with unwanted death and expulsion
of the fetus.
Induced abortion
When the pregnancy is terminated by
eliminating the fetus or embryo before it can survive outside the mother's
uterus.
Indirect abortion
When the
death of the fetus is caused during a medical intervention. This is
performed in two circumstances: when the mother's life must be saved or when
the viability of the fetus is nil.
Dangerous abortion
It is the termination of pregnancy
performed by people who do not have the necessary training and preparation
and/or is performed in an environment that does not meet the minimum medical
conditions.
Preventive measures
There is no effective preventive therapy
in the treatment of threatened miscarriage. However, weekly monitoring of the
pregnancy can be performed until the bleeding is resolved, and also pay
attention to the risk of preterm delivery, oligohydramnios, and intrauterine
growth restriction (Carbajal-Sánchez & Nery-Segura, 2018).
Threat
of abortion
According to Vasquez De La Torre (2018),
it is a dangerous situation with a risk of culminating in abortion before 20
weeks of gestation; It is characterized by scanty metrorrhagia, with or without
pain in hypogastrium type colic, closed cervix. Generally, ultrasound evidence
of intrauterine gestation with development is available according to
gestational age.
Likewise, a threatened abortion is
suspected when bloody vaginal discharge or frank Hemorrhage appears during the
first half of pregnancy. In this situation, out of 30 %, approximately half
miscarry (Gaspar-Huánuco & Torres-Rojas, 2018).
Finally, according to Huanca Morales
(2020) in the eCIE10ES (2022), threatened abortion is defined as specified
Hemorrhage as a consequence of threatened abortion.
Pathophysiology
According to Ocón-Cabria (2017),
threatened abortion is preceded by bleeding during the first trimester of
pregnancy, originating inside the uterus. Mainly, the bleeding is caused by the
embryonic implantation of the blastocyst in the internal wall of the
endometrium, initiating the formation of the placenta. In the first 20 weeks of
gestation, alterations (anatomical or physiological) or bleeding may occur,
mainly as a result of the formation of retrochorionic hematoma, which may
evolve favorably or culminate in miscarriage.
Also, these characteristics are
accompanied by colicky pain in the lower abdomen, which indicates the possible
case of spontaneous abortion, considered as uninduced embryonic or fetal death
before 20 weeks of gestation.
Risk Factors
There is evidence of a high frequency of
miscarriage incidence in the following cases: when the patient presents
anatomical uterine anomalies; when surgical correction has decreased the
incidence of first trimester losses, mainly in recurrent miscarriage; with the
presence of polyps larger than 2 cm, increased number and size of uterine
fibroids that hinder implantation and poor blood supply to the fetus; with the
appearance of tumors of rapid growth and degeneration with cytokine release,
submucosal location or total occupation of the uterine space that hinders the
growth of the fetus and uterine adhesions, although on this point more evidence
is needed. (Carbajal & Segura, 2018).
Etiology
According to Carvajal-Cabrera and
Barriga-Cosmelli (2021), threatened abortion is generally caused by chromosomal
(49 % of cases) and morphological abnormalities of the gametes, as well as
anatomical abnormalities of the maternal genital tract; endocrine diseases such
as corpus luteum insufficiency, hypothyroidism, hyperthyroidism and
uncontrolled diabetes mellitus; also, by systemic diseases and infections such
as syphilis, rubella and toxoplasmosis; by immunological factors; by ABO
incompatibility; by toxic factors with the use of folic acid antagonists and
lead poisoning; and by traumatic factors.
Clinical signs and symptoms
The clinical picture is based on the
history of transvaginal bleeding during the first 20 weeks of gestation,
evidencing the presence of a closed cervix, with or without uterine
contractions, secondary amenorrhea, positive pregnancy test (quantitative β-Hcg),
fetal vital activity, colicky pain in hypogastrium, uterine volume consistent
with amenorrhea, without dilatation or cervical modifications (Ochoa-Marieta et
al., 2018).
The presenting signs and symptoms are:
vaginal bleeding, usually scanty during the first 20 weeks of gestation; pain
in the back and lower abdomen. In most cases the vaginal bleeding stops on its
own and the pregnancy runs its course; in other cases the threat progresses to
miscarriage (Mayo Clinic Staff, 2020).
Treatment
Treatment depends on the results of the
ultrasound: if it shows ovarian viability, the results of quantitative β-Hcg
are in normal ranges and there is no active bleeding, so the respective
outpatient management and control should be performed in 72 hours, as well as
absolute rest, and metabolic, infectious or other causes should be treated.
Suppose there is a certain placental detachment, or the quantitative β-Hcg
tests express a specific hormonal deficit. In that case, the patient should be
hospitalized for control and evaluation of the pregnancy, with absolute rest,
and with administration of progestogens 100 mg. twice a day, discharge after 24
or 48 hours without vaginal bleeding, with rest at home and control within 7 to
10 days in the hospital outpatient clinic. If the ultrasound does not reveal a
positive embryo plaque, but the quantitative β-Hcg is positive, rest should be
prescribed, without medication (Ríos Canales et al., 2018).
In the pharmacological treatment of
progesterone injectable solution 50 mg every 48 hours as a support,
progesterone is used in cases of established luteal phase defect. In recurrent
abortion of unspecified etiology, and in patients who have received ovulation
inducers. The use of antispasmodic suppositories is limited, especially in the
period of organogenesis between 18 and 55 days post conception (ANAEL, 2015).
Complications
The most common complication is
miscarriage and anemia resulting from moderate or severe blood loss, which may require blood
transfusion; infection or the likelihood of ectopic pregnancy, which is a
potentially life-threatening complication, should not be ruled out
(Gaspar-Huánuco & Torres-Rojas, 2018).
Preventive measures
There is no effective preventive therapy
in the treatment of threatened miscarriage, which requires weekly monitoring of
the pregnancy until the bleeding is resolved and attention should be paid to
the risk of presenting preterm delivery, oligohydramnios and intrauterine
growth restriction (León et al., 2016)
Nursing role in the care of threatened abortion patients
The nursing role is primarily aimed at
monitoring and documenting the clinical progress of the patient at risk of
miscarriage. Nursing activities from this perspective can be developed when
knowledge and skills merge to reach sufficient understanding of the phenomenon
and its complexities. This requires ongoing psychological support for the
couple and family because emotional bonds develop as the gestation progresses
and are associated with feelings of failure in the pregnant woman. It is also
necessary to provide a quiet environment to rest, as sleep is vital for
recovery and improvement of the psycho-social balance (Cornejo-Sánchez, 2020).
In the case of a pregnant patient,
emotional support should be provided with the participation of the husband
and/or family, seek help to promote security and positive attitude; monitor the
color, odor and duration of bleeding; control the temperature of the pregnant woman
during the first week; avoid the use of tampons or vaginal douches for 15 days;
sexual abstinence during the first 15 days; consider general measures such as
absolute rest; and try to manage the emotional state of the patient (EAFIT,
2018).
Risk
of antepartum complication: hemorrhage
Vaginal bleeding in the first trimester
of gestation is a frequent situation that occurs between 15 to 25 % of all
pregnancies, putting the life of the mother and fetus at risk (Alayo-Huatay,
2019). According to Herdman and Shigemi (2019), this involves the risk of
bleeding, leading to a decrease in blood volume that can seriously compromise
health.
On the other hand, statistical data
indicate that maternal mortality is a health indicator that evidences social
exclusion, low accessibility to health services, gender inequity in
decision-making, little respect for human rights and limited access to health
services. 27,1 % indicates maternal death due to hemorrhage, according to the
recent Lancet 2014 review, which analyzed global, regional, and sub-regional
estimates of causes of maternal mortality during 2003-2009. In indigenous
populations, the maternal mortality rate is 25 % across the board. Abnormal
genital bleeding should be classified as a priority, assessing the amount and
rate of immediate postpartum blood loss in the first 24 hours postpartum (INEI,
2019).
Causes
Taking into account Bunce and Heine
(2020), hemorrhage in the first half of pregnancy will depend on whether the
pregnancy is ectopic, tubal, or cervical; in 1,5-2 % of these cases, blastocyst
implantation occurs outside the uterine cavity. The most frequent location is
in the fallopian tubes (98 % of cases). It can also occur at the cervical
level, in the ovary, in the pelvic cavity, and even in the abdominal viscera.
Treatment
Clinical management will depend on the
amount of bleeding, the gestational age, and the type of placental
implantation. In the event of presenting hemorrhage, the lost blood is replaced
immediately, and a transfusion is administered as a priority while the
emergency is resolved; in this situation, it is essential to stop the bleeding
and eliminate its origin. In the face of acute bleeding, expansion with plasma
is preferred rather than with solution (Llanos-Cerquín, 2018).
On the other hand, surgical treatment
consists of the removal of placental remains and the respective repair of
genital lacerations or uterine curettage (MINSA-CSS, 2015).
Likewise, complementary treatment
includes the administration of uterotonic drugs with oxytocin, prostaglandins,
methylergonovine, and fluid replacement or transfusion, iron supplementation,
clinical control, and ultrasound monitoring (Carvajal & Barriga, 2021).
Complications
In the process of threatened abortion,
bleeding is an emergency complication that must be treated immediately, with
the respective pharmacological treatment to control the hemorrhage, and the
application of uterine massage to stimulate contraction and avoid abundant
bleeding blood discharges. In addition, the respective blood transfusion is
recommended to replace losses that could lead to significant complications. If
care is not timely or there is little expertise in the prevention of these
complications, the probability of death of the pregnant woman is 100 %; therefore,
in order to maintain hemodynamics, a constant blood volume needs to be
relatively preserved (Alayo-Cuzcano et al., 2018).
Prevention
Preventive measures for hemorrhage are
implemented through strict compliance with care protocols based on clinical practices
from patient admission to discharge, prioritizing respect for life,
confidentiality, and privacy.
There is no effective preventive therapy
in threatened abortion (Ochoa-Marieta et al., 2018).
Likewise, early identification of risk
factors, the work of the multidisciplinary team, and the initiation of
procedures that allow preservation of a safe intravenous line for volume
replacement are important. Also important is the strict control of vital signs,
assessment of signs of shock, assessment of fetal heartbeat, provision of a
blood bank, adequate positioning of arterial catheters for uterine
embolization, and placement of urethral catheters, all of which contribute to
the patient's good condition.
In addition, bed rest, abstinence from
sexual intercourse, decrease of tense emotions, and, in some cases, the use of
progesterone in the preparation of the uterus for implantation of the
fertilized egg are required (Neyra-Díaz & Palominpo-Bonifacio, 2019).
Nursing
care for bleeding
According to Rivero-Navia and
Pintado-Abad (2017), the following procedures are considered in the management
of uterine bleeding: monitoring of the patient's state of consciousness,
assessment of pupils, control of vital signs preferably every 15 minutes,
attention to changes in blood pressure, monitoring of uterine involution,
control and assessment of vaginal bleeding (scanty, moderate, abundant),
control and assessment of vaginal bleeding (especially the amount, color and
consistency), strict compliance with medical indications, accurate water
balance, assessment of the level of anxiety and fear of the patient and her
family, pain management and alertness to warning signs (confusion or altered
lucidity, pallor, cold and clammy skin), arterial hypotension, tachycardia,
weakness, bleeding greater than 500 ml, and shortness of breath.
Effective maternity process
Maternity in Peru has faced various
challenges, such as raising awareness and engaging and motivating public and
private entities on safe motherhood. For example, in 1988, the third week of
May was declared "Healthy and Safe Motherhood Week" in order to
prevent the death of the pregnant woman and/or her child during pregnancy,
childbirth or puerperium; the cultural and socioeconomic context was considered
as factors that influence the reproductive behavior of women and their
environment (UNFRA-Peru, 2021).
For its part, MINSA-CSS (2015) has
implemented care during pregnancy with at least six prenatal check-ups for
pregnant women; this includes breast exams and teaching breast self-examination
(prevention of breast cancer), breast sampling for pap smear and/or visual
inspection of acetic acid (prevention of cervical cancer), continuity in the
nutrition of the pregnant woman and the unborn child, counseling for early and
exclusive breastfeeding, and administration of micronutrients (iron, folic
acid, and calcium supplements).
Similarly, MINSA-CSS. (2015) includes
timely teaching in identifying warning signs, birth plan with the pregnant
woman, couple counseling, family counseling, community support, counseling and
guidance in HIV and syphilis pre-test, rapid test for HIV and syphilis,
assessment of cases of family or sexual violence, screening for depression,
detection of proteinuria in each visit in order to detect hypertensive/pregnancy
diseases, detection of urinary infections, detection of anemia, gestational
diabetes, analysis of blood group and blood factor, application of six sessions
of obstetric psychoprophylaxis with the participation of the couple and the
family, and the implementation of six sessions of obstetric psychoprophylaxis
with the participation of the couple and the community, detection of anemia,
gestational diabetes, blood group and blood factor analysis, six sessions of
obstetric psychoprophylaxis with the participation of the couple and the
family, six sessions of prenatal stimulation with the participation of the
couple, ultrasounds at the first visit and in the third trimester, two dental
exams, vaccinations against tetanus, influenza and others, three home visits,
and fetal monitoring once in the third trimester.
Ineffective maternity process (00221)
In 2012, MINSA recorded hemorrhage (40,2
%), followed by pregnancy-induced hypertension (32 %), abortion (17,5 %), and
various infections during the puerperium period (4,1 %) as causes of death.
Likewise, certain regions in the interior of Peru register high maternal
mortality figures, such as Lima, Cajamarca, La Libertad, Puno, Piura,
Lambayeque, Ancash, Arequipa, Callao, Apurímac, and Loreto.
According to Herdman and Kamitsuru
(2017), the process of ineffective mothering comprises the "inability to
prepare for and/or maintain a healthy pregnancy, birthing process, and newborn
care to ensure well-being" (p. 329). In the day-to-day work, the nursing
considers that the process of ineffective motherhood involves a set of specific
interventions aimed at the care of the pregnant woman and the fetus, which do
not match due to their vulnerability and biological, psychological, and social
factors, as well as failed compliance with norms and expectations.
Defining characteristics of ineffective childbearing
It is presented through specific
clinical manifestations, as evidenced by NANDA International, as detailed as
"inadequate access to support systems, inadequate prenatal care,
inadequate prenatal lifestyle, inadequate preparation of items for the newborn,
inadequate preparation of the home environment, ineffective management of
bothersome symptoms during pregnancy, unrealistic birth plan, and insufficient
respect for the neonate, among others" (Herdman & Shigemi, 2019,
p.329). However, in the case of the patient under study, this problem was
evidenced by fever, frowning, inadequate prenatal management, ineffective
management of bothersome symptoms during pregnancy, and inadequate prenatal
lifestyle.
Factors related to ineffective childbearing
The causal factors that the NANDA I
taxonomy considers are: "substance abuse, insufficient knowledge about the
childbearing process, insufficient prenatal care, insecure environment,
maternal helplessness, insufficient parental role modeling, inadequate maternal
nutrition, unrealistic birth plan, low maternal confidence, insufficient
cognitive preparation for parenting, insufficient support systems, maternal
psychological distress, domestic violence, and sporadic health provider visits
during pregnancy, among others" (Herdman & Shigemi, 2019, p. 329).
Following the above, it is worth mentioning that the patient presented an
ineffective maternity process due to insufficient prenatal care and inadequate
maternal nutrition.
For her part, Bruno-Maldonado (2019)
believes that ineffective motherhood usually occurs for different reasons, for
example when mothers do not have sufficient knowledge for their care, lack of
skills and resources necessary for the proper development of the motherhood
process, or due to incorrect conditioning in their environment or in the
characteristics of the process that hinder the proper development of the
maternal role. In addition, these factors include insufficient knowledge of the
motherhood process and lack of confidence, insufficient or non-existent support
systems, situations of unplanned or unwanted pregnancy, and even situations of
risk, social exclusion, or gender violence.
Nursing care in the process of ineffective childbearing
The contribution of nursing in maternal
care consists of educating and strengthening the pregnant woman in the
awareness of the value of health, in applying intervention and outcome
assessment procedures, and providing timely care that allows adequate
monitoring of the evolution of pregnancy (Herdman & Kamitsuru, 2017). Also,
it is necessary to highlight the role of the nursing professional by empowering
him/herself in the activities of accompaniment, education and counseling
through care such as: propitiating prenatal consultation that allows adequate
monitoring of the evolution of pregnancy, promoting safe motherhood, educating
about care and upbringing of the newborn, involving social participation that
contributes to the improvement of aspects of daily life, culture and political
activity related to health, fostering an intersubjective relationship with the
team of obstetrics, nursing and obstetric nursing professionals, pregnant woman
and family; all to reduce the risks of this physiological process (Herdman
& Kamitsuru, 2017).
Theories
of human care and adaptation
The nursing process, through the
scientific method, will test the validity of the theoretical nursing model
through research in practice. For the case under study, the theories of Jean
Watson and Callista Roy were taken as a frame of reference, in which human care
is centered on the person and the adaptation process is attended to (EAFIT,
2018).
The present work is based on Watson's
theory, "Theory of the philosophy and science of care" or
"Theory of human care," which allows assessing, identifying, and
evaluating human care; this is emphatically applied to the care to be provided
to the patient with threatened abortion, as it rescues the human aspect, spiritual,
and transpersonal sensitivity in clinical, administrative, educational, and
research practice in nursing (Cornejo, 2020).
Considering that the study deals with a
process of alteration in the mother-child binomial, three dimensions of
Watson's theory were chosen: first, health as a unity and harmony between body
and soul; second, the person as a unique being free to make decisions; and
third, the integral aspect, because the patient can participate in her care
considering her sociocultural, religious and emotional aspect (Neglia C.,
2017). Therefore, this theory allows for guiding care in a softened way,
sustained in a humanistic system, and integrating scientific knowledge in the
science of care to facilitate a better quality of life.
Likewise, the nursing work is identified
with the theory of the adaptation model of the theorist Callista Roy, because
in the case study it is considered that gestation is a process of constant
person-environment interaction that adapts to train coping mechanisms; this allows
highlighting the importance of her environment to survive in her conversion to
motherhood. In the same way, nursing work is emphasized in its focus on all
contexts of the patient: health, environment, well-being, etc. Therefore, in
this process, the patient will be able to be responsible for her care and play
new roles, and timely nursing intervention will lead to a higher level of
health and well-being (Pezantes-Lazo, 2018).
Finally, as mentioned by Álvarez-Maita
(2020) and WHO (2020), this practice promotes in health professionals a
humanized treatment of the person based on comprehensive training, proper
management of health services systems, and a safe communication system.
Therefore, this case study proposes activities that provide scientific, specialized
care, as well as philosophical, ethical, and moral bases to promote a better
quality of life in the mother-child binomial.
METHOD
Study
design
The present study consists of a research
with qualitative approach, with a type of study is single clinical case that is
based on the method of the Nursing Care Process (PAE), in order to answer the
objectives formulated in the study about the process of ineffective maternity
and the risk of hemorrhage complication in a patient with threatened miscarriage.
Subject
of the study
22-year-old female patient, on her
second day of care, selected at the convenience of the researchers, diagnosed
with threatened abortion at 11 weeks of gestation by ultrasound. According to
her state of vulnerability, manifestations of the process of ineffective
maternity and susceptible to hemorrhage were observed.
Scope
and period of the study
The study was conducted in the
obstetrics and gynecology service of the "Santa Rosa" National
Hospital in the Lima Region, from April 12 to 14, 2021.
Data
collection procedure
Source
of information
The following instruments were used:
verbal information provided by the 22-year-old patient M. R. V., direct
observation of the patient, clinical history, medical and nursing evolution
records and physical examination; likewise, these materials were admitted with
the assessment tables, applying the nursing assessment guide according to
Marjory Gordon's 11 functional patterns and the bibliographic review as
scientific evidence.
On the other hand, the review of
scientific evidence was carried out using the following databases: Science
Direct, Elsevier, Medline, and Scielo. In addition, documents from official
entities (WHO, American Cancer Society), MINSA, practice guides and protocols,
theses, and books on nursing were consulted. Interviews and observation were
also used for the collection and analysis of the information.
Information
procedure
To proceed with data collection, prior
authorization was obtained from the patient M. R. V. and the person in charge
of the gyneco-obstetrics service of the National Hospital "Santa
Rosa", Lima, guaranteeing, during the whole process, the protection and
confidentiality of the data provided for the realization of the study, with no
identifying information about her.
Collection of information
First phase
The patient's medical history was read
and reviewed to extract clinical data such as: personal and family history,
reason for consultation, test results, main medical diagnosis, medical and
clinical evolution, as well as the evolution of nursing care.
Second phase
A nursing assessment was performed
through a personal interview, following Marjory Gordon's 11 functional
patterns, using the identification and recognition of the main nursing
diagnoses for the development of a specific care plan focused on the case
study.
Third phase
The two follow-ups performed on the
patient were found in order to see the evolution of the same.
Fourth and final phase
An exhaustive review of the scientific
evidence was carried out, setting limits according to date criteria, from 2016
to the present. Likewise, some databases were used such as: Science Direct,
Scielo, Elsevier, Google Scholar, and keywords such as: nursing role, care,
patient and threat of miscarriage.
Data processing
The data were analyzed and organized
based on nursing methodology, following the following procedures:
An analysis was performed based on the
nursing methodology associated with the AREA model of Pesut and Herman (2019).
After assessing the patient based on the 11 Marjory Gordon functional patterns,
a clinical reasoning network was performed based on the aforementioned model to
select the primary nursing diagnosis with the taxonomy (NANDA International,
2018). Then, after the choice of the DxEp, we proceed to the establishment of
the expected outcome criteria (NOC) and nursing interventions (NIC) and the
respective activities.
A critical analysis of the scientific
evidence included in this study was performed, taking as a basis the objectives
raised according to NOC taxonomy (Moorhead et al., 2019) and prioritizing it
with the AREA model (Pesut & Herman, 2019), in order to obtain the central
NOC of the nursing diagnosis and the main collaborative problem; this has an impact
on the preparation of the respective care plan having the NIC taxonomy as a
basis (H. Butcher et al., 2018).
The programmed nursing activities were
carried out, with subsequent evaluation of the same to verify the degree of
effectiveness of the interventions carried out according to the patient's
individualized care plan.
RESULTS
Case
description
Young adult female patient, 22 years
old, from the La Victoria, Lima district. She was admitted to the emergency
gynecology department of the hospital at 09:00 am, accompanied by her husband.
She was seated in a wheelchair, flexed on her knees. She was thin, in good
hygienic condition, and reported that she felt very weak and 2 days ago she
presented brown bloody stains in her vagina, which increased. She was fearful,
very sleepy, and unable to stand up. She reported that the night before, she
could not sleep, perhaps because of her constipation, plus nausea and vomiting
for 3 days, with a very painful and swollen lower abdomen. His additional
concern was his intention to go to work.
Nursing
Care Process
Valuation
Marjory Gordon's 11 function patterns
were used for the assessment.
Description
of functional health patterns Functional pattern 1. Perception health
management Altered pattern
Patient in REG, with good hygienic
conditions, from the district of La Victoria, Lima. She is 11 weeks pregnant,
without pre natal control, unaware of pregnancy. She does not receive
medication. With medical diagnosis: threatened abortion and 11 weeks gestation
by ultrasound. She has had amenorrhea for more than two years (hormonal
contraceptive injectable every three months). She had her first pregnancy three
years ago (euthyroid delivery and at term), she underwent abdominal ultrasound.
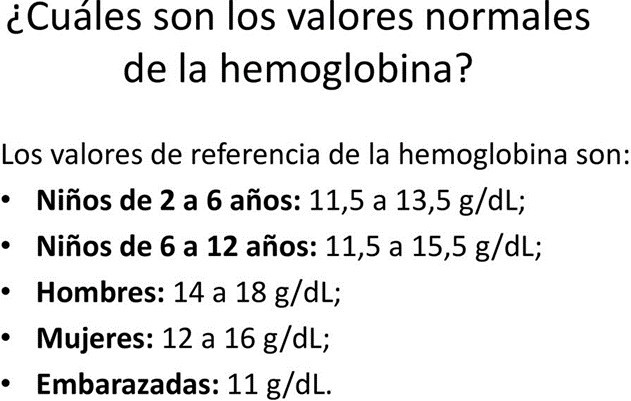
She denied previous abortion and allergies. With hemoglobin level of 10,5
mg/dl, as a result of beta-human chorionic gonadotrophin (beta-hCG)
quantitative subunit of 13800. She received three doses of tetanus vaccine in
her first pregnancy.
Current
medical diagnosis
Threatened miscarriage and 11-week
gestation by ultrasound. Medical therapy:
Diet: NPO
Vital signs check every 30 minutes for 2
hours, then every hour, Bleeding check
Absolute rest
Parenteral hydration Cl. Na. 0,9 0/0, VE
at 40 gts x' OSA
Blood count control at 12 hours
Auxiliary tests
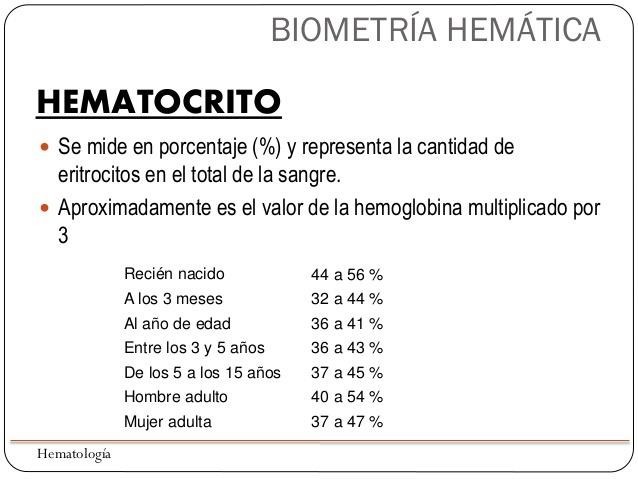
Laboratory results show:
Hemoglobin 10,5 mg/dl, VN: (13 mg/dl -
14,9 mg/dl) Hematocrit 31,4mg/dl, VN: (45mg/dl to 55mg/dl) Glucose 104mg/dl,
VN: (70mg/dl - 110g/dl)
Creatinine 0,61 mg/dl, VN: (0,6 mg/dl to
9,1mg/dl) Urine test: pH of 7,3 VN: (pH 7,35 - 7,45) VDRL test (-)
HIV test (-)
Blood group "O" and Rh (+)
Bleeding time of 2 minutes and 30
seconds. VN: (1 to 9 minutes) Clotting time of 30 seconds. VN: (25- 35 seconds)
Beta-quantitative subunit of VN: (11500-289000 mIU/ml:) human chorionic
gonadotropin.
(beta-hCG) of 13800
Abdominal ultrasound: thickened uterine
wall and presence of an embryo sac of approximately 11 weeks.
Functional pattern 2: Metabolic Nutritional
Altered pattern. BMI: 23,04 (normal
weight), skin and mucous membranes pale and semi-hydrated, afebrile, abdomen
painful on palpation, nauseous sensation and vomiting three days ago and
constipation.
Functional pattern 3: Elimination
Altered pattern. Constipation three days
ago.
Functional pattern 4: Activity and exercise
Altered pattern. P. A of 90/50mmgHg, HR
of 125 per minute, FR of 20 per minute, difficulty sleeping, sitting in
wheelchair due to pain, in semi-flexed position and weakness.
Functional pattern 5: Rest and sleep
Altered pattern. She reported not
falling asleep, with pain and weakness, unable to stand, sitting in a wheelchair.
Functional pattern 6: Cognitive perceptual
Altered pattern. Patient lucid, oriented
on PET, with lower abdominal pain.
Functional pattern 7: Self-perception - self-concept
Effective Employer. Worried because she
does not attend work. She feels fearful and has not been able to sleep for
three days.
Functional pattern 8: Role - Relationships
Altered pattern. She has accompaniment
and support from her partner. She generates her own income. She has a three-year-old son. She is concerned about
her absence from work.
Functional pattern 9: Sexuality - reproduction
Altered pattern. Two gestations, had a
euthyroid delivery two years ago. She did not receive CPN. FUR two years ago
(used injectable contraceptive every three months). Asymmetrical breasts,
nipple and areolas dark, turgid, without secretions, without presence of striae
or masses. Uterus not palpable, very sensitive to palpation. Genitalia of
normal appearance with presence of dark brown discharge, in small quantity in
the sanitary napkin. No amniotic fluid leakage. Second stage of pregnancy at
eleven weeks by ultrasound, menarche at 13 years of age. Sexual debut at 16 years of age.
Functional pattern 10: Adaptation to stress tolerance
Effective employer. Concern about her
job, as she will miss the days she remains in the hospital. She is a contracted worker.
Functional pattern 11: Values and beliefs
Effective employer. Practitioner of the
evangelical religion.
Care
plan
Diagnosis
The formulation of nursing diagnoses
(DxE) was performed according to the NANDA International taxonomy (Herdman
& Kamitsuru, 2017).
Functional pattern 1: Perceived health management
(00043) Ineffective protection r/w
inadequate nutrition m/p weakness, immobility and insomnia.
Definition: "Decreased ability to
self-protect from internal and external threats such as illness or injury"
(Herdman & Kamitsuru, 2017, p. 160).
Domain
1: Health promotion
Class
2: Health management
Functional pattern 2: Metabolic Nutritional
(0002) Nutritional imbalance: intake
below requirements r/insufficient food intake m/p inability to ingest food,
pallor of mucous membranes, abdominal pain, insufficient muscle tone.
Definition: "Insufficient nutrient
intake to meet metabolic needs" (Herdman
& Kamitsuru, 2017, p. 171).
Domain
2: Nutrition
Class
1: Ingestion
Functional pattern 3: Elimination
(00011) Constipation r/c pregnancy m/p
abdominal pain, inability to defecate and vomiting.
Definition: "Insufficient nutrient
intake to meet metabolic needs" (Herdman
& Kamitsuru, 2017, p. 215).
Domain
3: Elimination and exchange
Class
2: Gastrointestinal function
Functional
pattern 4: Activity and exercise
(00085) Impairment of physical mobility r/pain and decreased
strength muscular m/p gait disturbance, postural instability, limited range of
motion and difficulty in standing.
Definition: "Limitation of
purposeful independent movement of the body, of one or more limbs"
(Herdman & Kamitsuru, 2017, p. 239).
Domain
4: Activity/rest
Class
2: Activity and exercise
Functional pattern 5: Rest and sleep
(00096) Of sleep deprivation r/c
prolonged discomfort m/p increased sensitivity to pain, discomfort and worry.
Definition: "Prolonged periods of
time without sleep (pattern of natural and periodic suspension of
consciousness)" (Herdman & Kamitsuru, 2017, p. 231).
Domain
4: Activity/rest
Class
1: Sleep/rest
Functional Pattern 6: Perceptual Cognitive
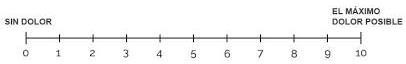
(00132) Acute pain r/c biological injury
agent m/p rating 7 according to VAS scale, verbal expression of pain in
hypogastrium.
Definition: "Unpleasant sensory and
emotional experience caused by actual or potential tissue injury or described
in such terms, of sudden or slow onset, of any intensity from mild to severe,
with a foreseeable end and a duration of less than 3 months" (Herdman
& Kamitsuru, 2017, p. 468).
Domain
12: Comfort
Class
1: Physical comfort
Functional pattern 8: Role - relationships
(00146) Anxiety m/p threatened by
current state r/c with insomnia, preoccupation with changes in life events,
fearfulness, increased heart rate and weakness.
Definition: "Vague, uneasy feeling
of discomfort or threat accompanied by an autonomic response (the origin that
is often nonspecific or unknown to the person); feeling of apprehension caused
by anticipation of danger. It is a warning signal that warns of impending
danger and allows the person to take action to deal with the threat"
(Herdman & Kamitsuru, 2017, p. 352).
Domain
9: Coping/stress tolerance
Class
2: Coping response
Functional pattern 9: Sexuality - reproduction
(00221) Ineffective maternity process
r/c with insufficient prenatal care, inadequate maternal nutrition m/p
inadequate prenatal management, ineffective management of bothersome symptoms
during pregnancy, and inadequate prenatal lifestyle.
Definition: "Inability to prepare
for and/or maintain a healthy pregnancy, birthing process, and newborn care to
ensure well-being" (Herdman & Kamitsuru, 2017, p. 329).
Domain
8: Sexuality
Class
3: Reproduction
(00209) Risk of maternal/fetal dyad
disruption r/c with inadequate prenatal care.
Definition: "Susceptible to
disruption of the maternal-fetal symbiotic relationship as a result of comorbidity
or pregnancy-related conditions that may compromise health" (Herdman &
Kamitsuru, 2017, p. 327).
Domain
8: Sexuality
Class
3: Reproduction
(00145) Risk of posttraumatic syndrome
r/c insufficient social support, environment not conducive to needs and
perception of the event as traumatic.
Definition: "Inability to prepare
for and/or maintain a healthy pregnancy, birthing process, and newborn care to
ensure well-being" (Herdman & Kamitsuru, 2017, p. 229).
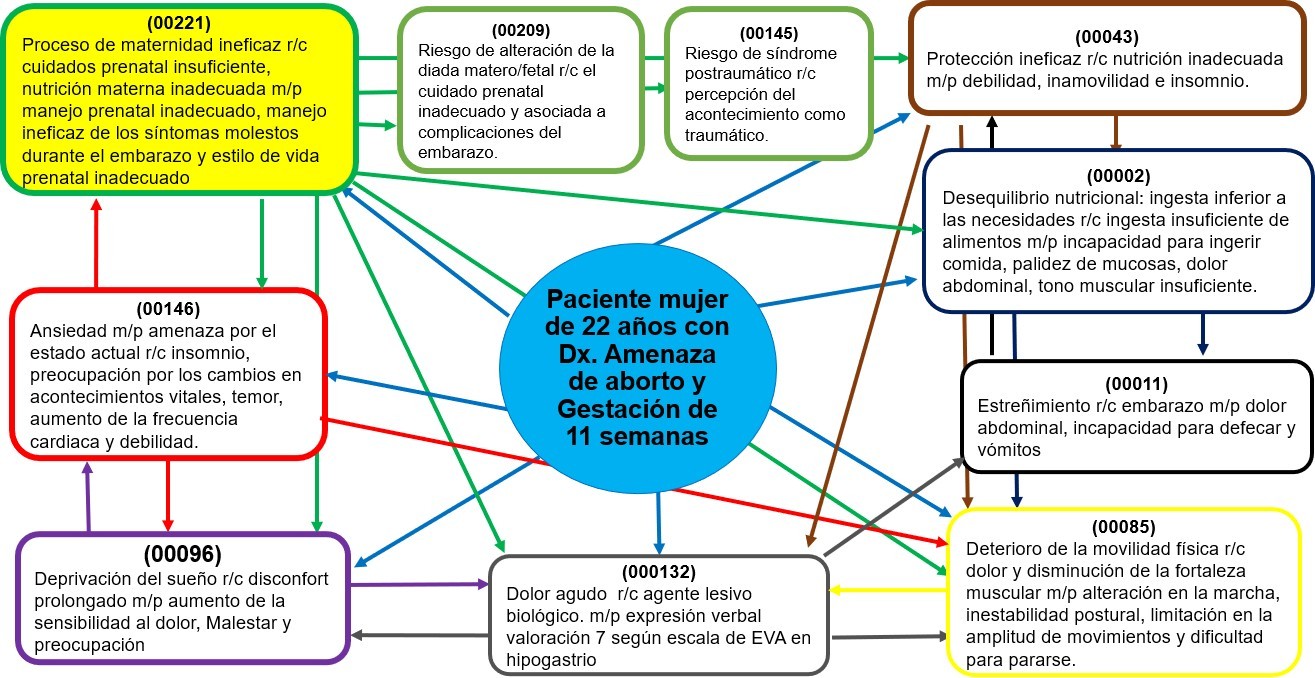
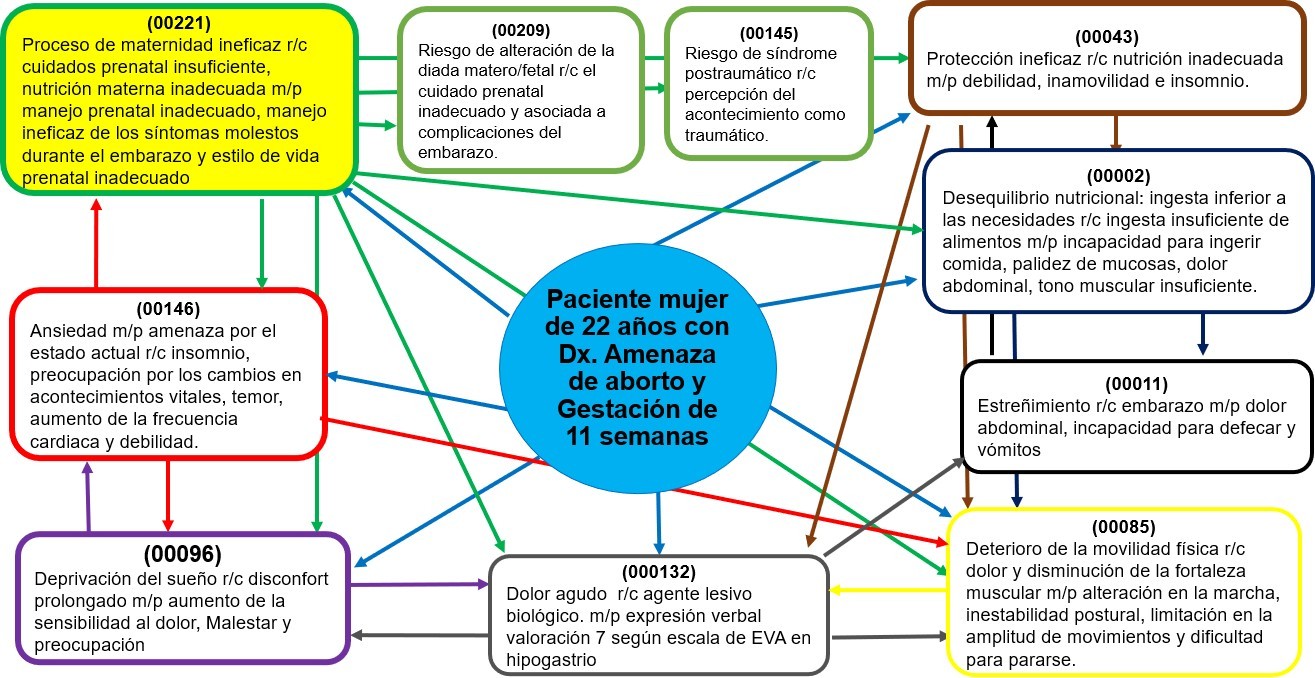
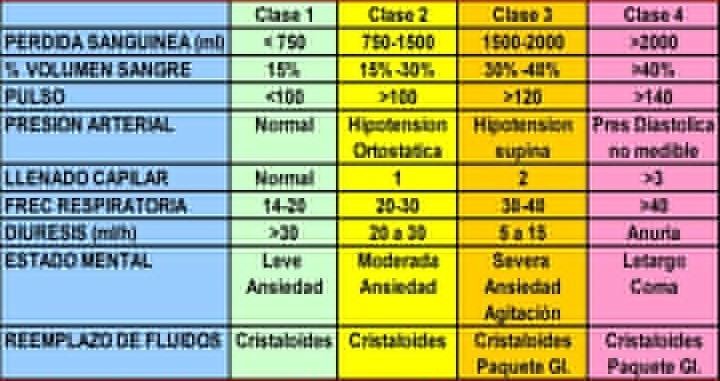
Figure 1. Critical reasoning
network, based on the AREA model for obtaining the main Dx.E
Main diagnosis
As can be seen in the Reasoning Network
(figure 1), the main DxE. is: (00221) Ineffective maternity process r/c with
insufficient prenatal care, inadequate maternal nutrition m/p inadequate
prenatal management, ineffective management of bothersome symptoms during
pregnancy and inadequate prenatal lifestyle.
Definition
"Inability to prepare for and/or
maintain a healthy pregnancy, birthing process, and newborn care to ensure
well-being" (Herdman & Kamitsuru, 2017, p. 329).
Domain
8: Sexuality
Class
3: Reproduction Justification of the main DxE
Fuertes Moreno (2019) mentions that
motherhood is a complex and personally transformative process, as it helps
pregnant women form bonds with their baby, partner, and family. In this period,
the threat of miscarriage can occur, which consists of a state that suggests
that a miscarriage could occur, and usually happens before 20 weeks of
pregnancy. It usually manifests with pain in the back and lower abdomen.
On most occasions, the vaginal bleeding
stops on its own and the pregnancy continues; however, at other times the
threat may progress to miscarriage. This process of ineffective childbearing
results in a degree of inability to prepare for and/or maintain a healthy
pregnancy, delivery, and newborn care.
On the other hand, it is important to
consider the relevance of Carvajal-Cabrera and Barriga's -Cosmelli (2021)
statement states that motherhood is often a positive experience; however, for
other women, it is synonymous with suffering, illness, and even death.
To conclude, in a process of ineffective
maternity, a complication is the threat of miscarriage that generates states of
anxiety, defined as an anticipation of future harm or misfortune, accompanied
by a feeling of dysphoria and/or somatic symptoms of tension. In this sense, it
is often better to observe the patient and assess their respective emotional
and behavioral manifestations, since these influence the course of the disease
(Carvajal-Cabrera & Barriga-Cosmelli, 2021).
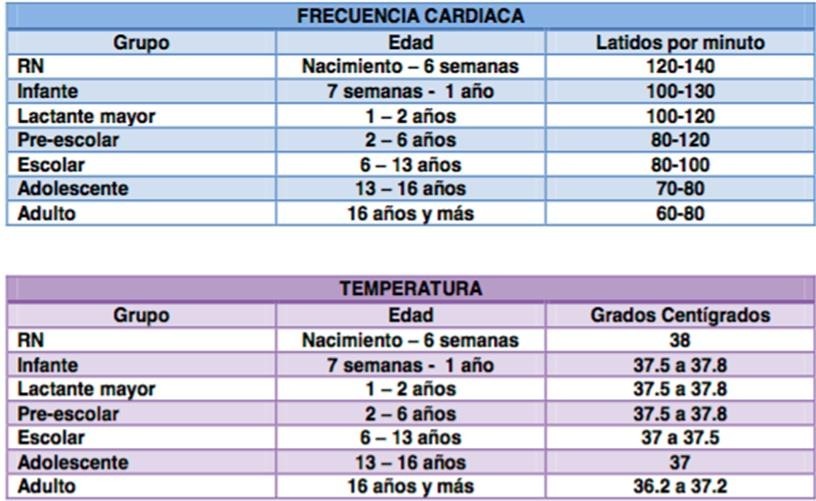
Collaboration problems (CP)
and their complication risks (CR)
In order to know which are the
collaborative problems (CP), as well as the patient's complication risks (CR),
the "Manual de Diagnósticos Enfermeros" by González-Aguña and
Santamaría-García (2015) was used.
Collaboration problem in pre-labor
period: CR Hemorrhage.
CR
Infection CR Acute pain
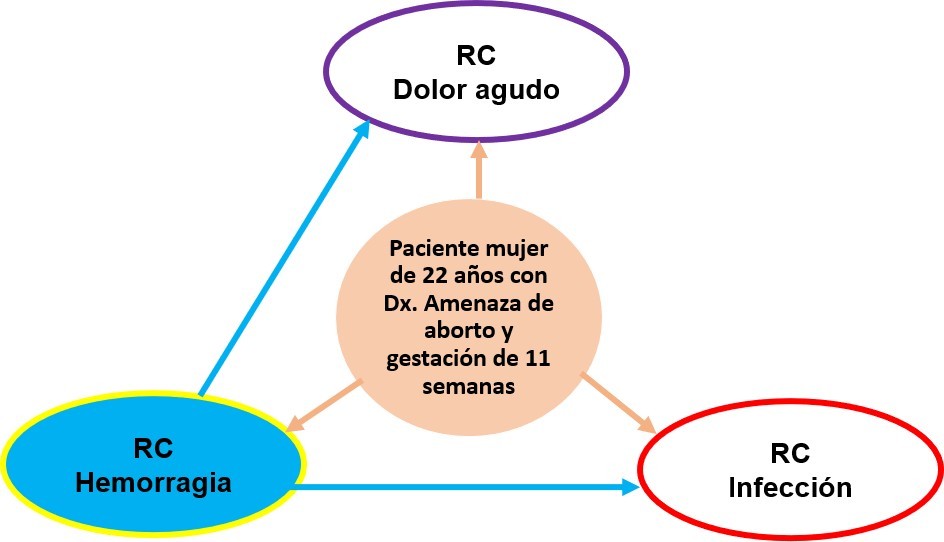
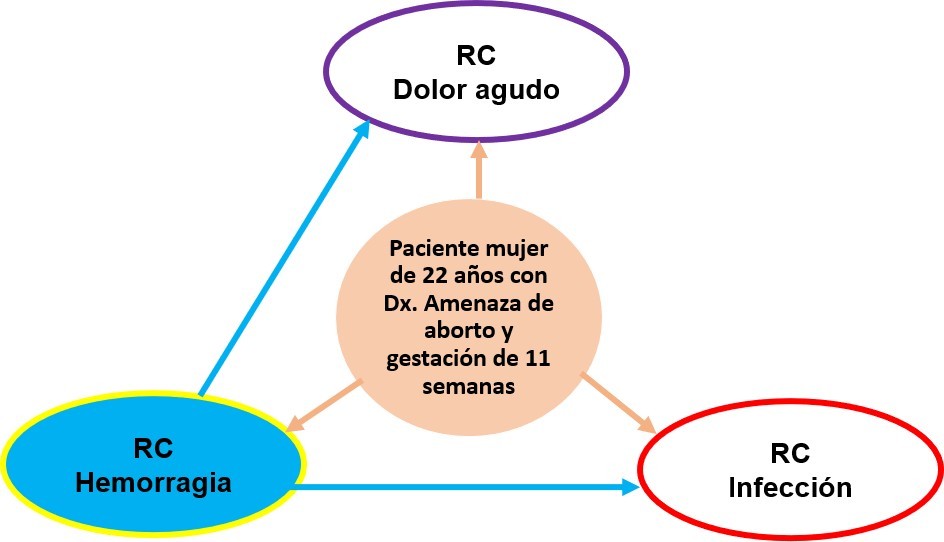
Figure 2. Critical reasonng
network based on the AREA method for obtaining the main complication risk (CR)
Identification of the main CR
CR hemorrhage has been identified as the
main complication risk, since it is the one with
the most arrows in relation to the others, being linked to CR acute pain
and CR infection.
CR Hemorrhage
Definition. Hemorrhage is the outflow or
loss of blood volume, inside or outside the body, due to rupture or injury of
one or more blood vessels, which causes a decrease in blood pressure; that is,
the heart increases its activity considerably in an attempt to raise its
cardiac output and conserve the volume of circulating blood. It is considered a
medical emergency; the severity depends on how fast, how much blood is lost,
and the patient's age. This continuous bleeding can lead to complications such
as anemia, hypovolemic shock, etc. (Bunce & Heine, 2020).
Justification of the main CR
In cases of post-threatened abortion
hemorrhage, timely intervention by the nurse is important, assessing the site,
amount, and rate of blood loss and the application of life support measures,
correctly recording the origin of the bleeding, noting the gestational age, and
identifying the differential diagnosis. Profuse bleeding is classified as a
priority in a frequent situation before the 20th week of gestation, occurring
in 15-25 % of all pregnancies. This puts the life of the mother and fetus at
risk (Ochoa, Reus, & Rogel-Cayetano, 2018).
On the other hand, the presence of
hemorrhage of intrauterine origin manifests with or without uterine
contractions, without cervical dilatation, and expulsion of the products of conception.
The care provided by the nurse in the case of hemorrhage is focused on the
patient with the aim is to prevent the onset of bleeding and promptly assess
the signs and symptoms of complications. To do this, activities will be
performed vital signs charting, assessment of strict body hemodynamics in the
water balance sheet, decreasing anxiety, preserving absolute rest, teaching
about the disease process and explaining alarm signs and symptoms, as well as
verifying the records of the annotations in the care plan, reports and updating
the Kardex and detailed examination of the incident in the nursing notes sheet
(NANDA, 2018-2020).
Similarly, it is important to focus on
the prevention of bleeding complications since bleeding is a sign that
expresses a decrease in blood volume, affecting cardiac output in relation to
the amount and frequency of bleeding. Timely intervention by the nurse is
important to avoid irreversible damage to the mother and the product of
conception (MINSA, 20|15).
It is also important to frequently
assess the patient's health, primarily when it is associated with acute
visceral pain and is accompanied by vegetative manifestations such as nausea,
vomiting, sweating, tachycardia, and increased blood pressure. When there is
tissue damage, it should be considered that, during gestation, estrogenic
hormonal changes and changes in the woman's pH (low acidity) occur, making her
susceptible to infection (Mayo Clinic Staff, 2020).
In conclusion, hemorrhage is a sign that
expresses a decrease in blood volume affecting cardiac output, including the
amount and frequency of bleeding. In this case, timely intervention by the
nurse is important to constantly assess the patient's health. Similarly, when
associated with acute visceral pain, it is accompanied by vegetative
manifestations such as nausea, vomiting, sweating, tachycardia, and increased
heart rate.
Blood pressure. As a sign of tissue
damage, it should be considered that, in the process of gestation, estrogenic
hormonal changes and changes in pH (low acidity) occur, which sensitize her to
infection (Bunce & Heine, 2020).
Blood pressure. As a sign of tissue
damage, it should be considered that, in the process of gestation, estrogenic
hormonal changes and changes in pH (low acidity) occur, which sensitize her to infection (Bunce & Heine, 2020).
Planning
Planning of the main nursing diagnosis (Dx.E.p)
To prevent and minimize the problem
presented in the patient, outcomes were determined and a set of interventions
were chosen as part of the care plan. The NOC (Moorhead et al., 2019) and NIC (Butcher et al., 2019) manuals of
objectives or outcomes were used.
DxE. main
(00221) Ineffective maternity process
r/c with insufficient prenatal care, inadequate maternal nutrition m/p
inadequate prenatal management, ineffective management of bothersome symptoms
during pregnancy, and inadequate prenatal lifestyle.
Definition
"Inability to prepare for and/or
maintain a healthy pregnancy, birthing process, and newborn care to ensure
well-being" (Herdman & Kamitsuru, 2017, p. 329).
Domain
8: Sexuality
Class
3: Reproduction
Outcomes (NOC) of the main nursing diagnosis
The NOC taxonomy responds to the patient
outcomes that are being sought, using
4-digit codes and six-digit indicators. For DxE. (0221) Ineffective
childbearing process, the following NOCs apply:
(1607) Prenatal health conduct
(1638) Knowledge: gestation (0111)
Prenatal fetal stage
(2006) Maternal prepartum personal
health status NOC prioritization of principal nursing diagnosis.
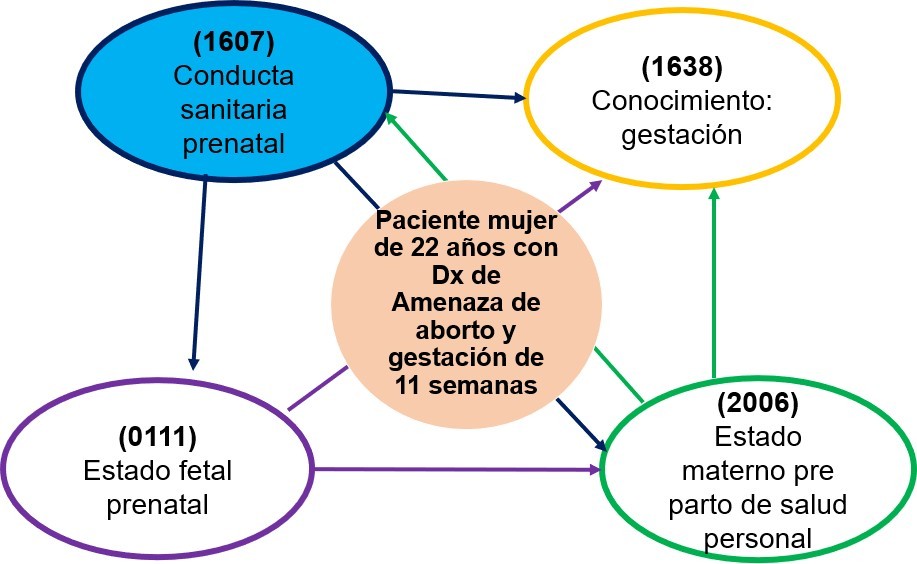
The analysis was carried out using the
critical reasoning network to define the main NOC. As shown in figure 03.
Figure 3. Prioritization of the
NOC of the main DxE by critical reasoning network based on the AREA method
Justification of the main DxE. main NOC
We can observe that according to the
critical reasoning network the main NOC corresponds to the one most related to
the other NOCs:
(1607) Prenatal Health Behavior
Definition: "Personal actions to
promote a healthy gestation and healthy newborn." (Moorhead et al., 2019,
p. 185).
Domain IV: Health knowledge and
behavior. Class Q: Health behavior.
The objective is related to improving
the maternity process and fetal well-being, as well as maintaining the
viability of gestation and at the same time preventing the risk of maternal and
perinatal morbimortality, because the approach has as a priority to maintain a
health behavior during the gestational period and therefore of the other
objectives and outcomes. In this sense, De la Herrán et al. (2018) consider it important
to know and deepen prenatal education to improve childcare policies,
reproductive care, and forms of parenting with preventive and interdisciplinary
plans. A lower blood supply to the fetus could cause fetal death.
|
Table 1. Main
NOC score for Dx.E.p.(Likert scale: 1-Never demonstrated. 2-Rarely
demonstrated. 3-Sometimes demonstrated. 4-Frequently demonstrated. 5-Always
demonstrated)
|
|
NOC
|
Initial Score
|
Target score
|
Time
|
|
(1607)
Prenatal Health Behavior
|
3
|
5
|
24 hours
|
|
Table 2. Scoring
of the Main NOC indicators, according to Likert scale (Likert scale: 1-Never
demonstrated. 2-Rarely demonstrated. 3-Sometimes demonstrated. 4-Frequently
demonstrated. 5-Always demonstrated)
|
|
Indicators
|
Initial score
|
Target score
|
Time
|
|
(160703)
Maintains visits of prenatal care
|
1
|
5
|
24 hours
|
|
(160710)
Maintains adequate nutrient intakes for gestation.
|
2
|
5
|
24 hours
|
|
(160723)
Uses supplements iron
|
1
|
5
|
24 hours
|
|
(160714)
Avoid exposure to infectious diseases.
|
2
|
4
|
24 hours
|
|
(160721)
Uses prescription medications
|
1
|
5
|
24 hours
|
Interventions (NIC) of the main Dx.E
To obtain the prioritized outcome, the
Nursing Intervention Classification (NIC) taxonomy was used.
(6680) Vital signs monitoring (Butcher et al., 2018, p. 341).
Definition: Collection and analysis of
data on cardiovascular, respiratory and body temperature status to determine
and prevent complications.
Domain
4: Safety
Class:
V Risk control Activities
(668001) Monitor blood pressure, pulse,
temperature, and respiratory status. (668002) Observe
blood pressure trends and fluctuations.
(668003) Monitor respiratory rate and
rhythm (depth and symmetry).
(668004) Monitor pulse oximetry.
(668005) Periodically monitor skin
color, temperature and moisture.
(4150) Hemodynamic regulation (Butcher et al., 2018, p.
393).
Definition:
Optimization of frequency, preload and cardiac contractility Domain 2: Complex
physiological
Class
N: Control of tissue perfusion. Activities
(415001) Perform a thorough assessment
of hemodynamic status (check blood pressure, heart rate, pulses, venous
pressure).
(415002) Recognize the presence of early
warning signs and symptoms indicative of hemodynamic system compromise.
(415003) Determine perfusion status
(indicate whether the patient is cold, warm or hot).
(415004) Monitor intake and output, diuresis, and
patient weight (1450) Management of nausea (Butcher et al., 2018, p. 296)
Definition: prevention and relief of nausea.
Domain
1: Basic physiological
Class
E: Promotion of physical comfort. Activities:
(145001) Monitor the effect of treatment
of nausea.
(145002) Encourage the patient to
control her own experience of nausea. (145003) Encourage adequate rest and
sleep to facilitate relief of nausea. (145004) Encourage eating small amounts
of food that is appealing to the patient. (145005) Encourage the patient to eat
small amounts of food that is appealing to the patient. (145005) Encourage the
patient to eat small amounts of food that is appealing to the patient a person
with nausea.
(145005) Weigh the patient regularly.
Functional pattern 9: Sexuality - reproduction
Concerning the first interview, a
notable decrease in dark brown vaginal bleeding was observed, continuing with
her 11-week pregnancy. Due to the transitory situation and the risk of
hemorrhage, it is difficult to predict that it will recur in the coming weeks.
For now, positive changes have been observed in the evolution of the process of
ineffective maternity in the face of the probability of presenting hemorrhage
and spontaneous abortion.
Finally, with the continuity of care
plan, the evolution and risk of hemorrhage are assessed, thus achieving the
greatest possible benefit.
Major
Complication Risk Planning (RCp) Hemorrhage
NOC
In order to determine the changes in the
patient's condition, the health outcomes measurement classifier was used
through NOC objectives (Moorhead et al., 2019). In terms of improving the
patient's quality of life, the NIC interventions were used (Butcher et al.,
2018). Consequently, the primary complication risk is CR Hemorrhage.
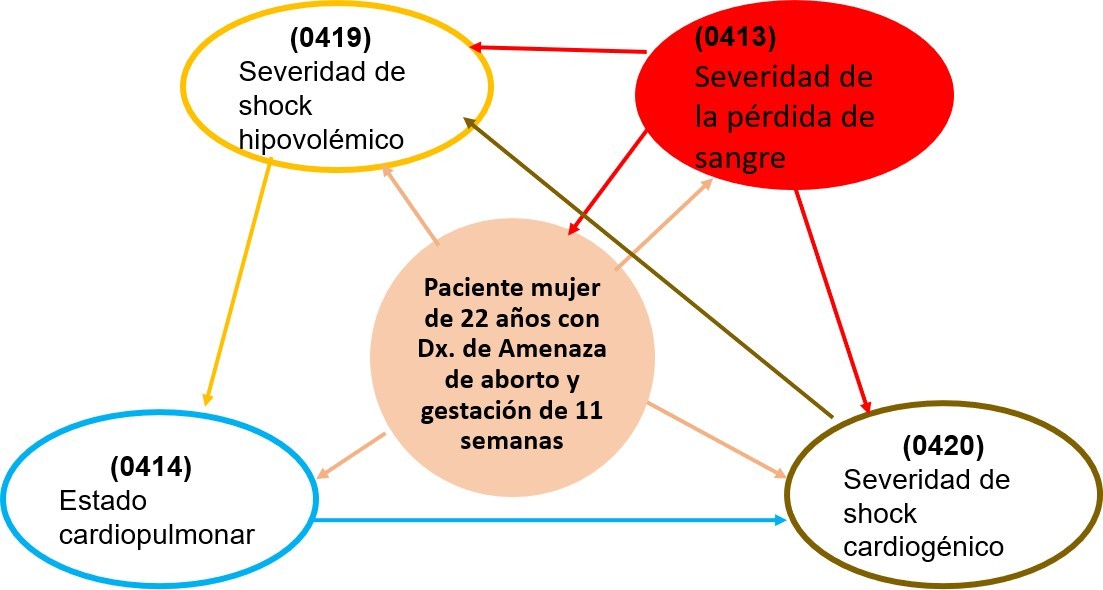
NOC results of the RCp
The NOC taxonomy responds to the
patient's desired outcomes, using 4-digit codes and six-digit indicators. The
following NOCs correspond to the CR Hemorrhage:
(0413) Severity of blood loss
(0419) Severity of hypovolemic shock
(0414) Cardiopulmonary status
(0415) Severity of hypovolemic shock
(0416) Severity of hypovolemic shock (0416) Cardiopulmonary status
(0420) Severity of cardiogenic shock
Figure 4. Prioritization of the
NOC of the main CR by Critical Reasoning Network Based on the AREA Method
Justification of the main NOC of the main CR
The severity of blood loss in
hemorrhages is variable and will depend on gestational age, pain intensity, and
possible labor. It can also occur as a result of placenta previa, premature
detachment of the placenta or uterine rupture; the risks increase if there are
risk factors such as: being older than 35 years, multiparous, previous cesarean
sections, pelvic diseases, history of uterine curettage, consumption of
addictives, etc. (MINSA, 2018). Therefore, it is concluded that maternal
hemorrhage is an emergency that should be treated as a priority, since it can
cause sudden loss of life (the fetus) and be the leading cause of maternal
death.
Prioritized
NOC of the CR Hemorrhage
(0413) Blood loss severity
Definition: "Severity of signs and
symptoms of internal or external bleeding." (Moorhead et al., 2019, p.
564).
Domain
II: Physiological health
Class
E: Cardiopulmonary
|
Table 3. Main
NOC score of CR Hemorrhage, according to Likert Scale (1-Severe. 2-Substantial.
3-Moderate. 4-Leve. 5-None)
|
|
NOC
|
Initial Score
|
Target score
|
Time
|
|
(0413)
Blood loss severity
|
4
|
5
|
48 hours
|
|
Table 4. NOC
Main NOC Indicator Scores for CR
Hemorrhage (Likert Scale: 1-Severe. 2-Substantial. 3-Moderate. 4-Level.
5-None)
|
|
Indicators
|
Initial Score
|
Target score
|
Time
|
|
(041307)
Vaginal bleeding
|
4
|
5
|
6 hours
|
|
(041313)
Pallor of skin and mucous membranes
|
3
|
5
|
6 hours
|
|
(041306)
Abdominal distention
|
3
|
5
|
6 hours
|
|
(041316)
Decreased hemoglobin (Hb)
|
3
|
5
|
6 hours
|
|
(041317)
Decreased hematocrit (Hto)
|
3
|
5
|
6 hours
|
|
(041314)
Anxiety
|
4
|
5
|
48 hours
|
|
(041309)
Decrease in systolic blood pressure
|
4
|
5
|
6 hours
|
|
(041310)
Decrease in diastolic blood pressure
|
4
|
5
|
6 hours
|
|
(041312)
Loss of body heat
|
4
|
5
|
6 hours
|
NIC
Interventions
(CIN) for risk of major complication (RCp)
Regarding the health behavior to be
followed in the prenatal period, it is necessary to perform in-hospital work
and counseling, which should then be performed by the patient at discharge. To
achieve the prioritized outcome, the Nursing Intervention Classification (NIC)
taxonomy was used.
Risk
of major complication (RCp). Hemorrhage
(4010) Hemorrhage prevention
Definition: "Decrease in stimuli
that can induce bleeding in patients at risk for bleeding" (Butcher et
al., 2019, p. 377).
Domain
2: Complex physiological
Class
N: Control of tissue perfusion
(441001) Monitor the patient closely for
signs and symptoms of internal or external bleeding (e.g., abdominal swelling).
(441002) Record hemoglobin and
hematocrit levels, before and after blood loss, as indicated.
(441003) Maintain intravenous access.
(441004) Maintain bed rest during active
bleeding.
(441005)
Instruct patient and/or family on signs of bleeding.
(5310) Give hope.
Definition: "Increasing belief in
one's own ability to initiate and sustain actions" (Butcher et al., 2019,
p. 158).
Domain
3: Behavioral.
Class
R: Coping assistance
(145001) To help the patient and family
identify areas of hope in life. (145002) To foster therapeutic relationships
with loved ones.
(145003) Assist the patient in designing
and reviewing goals related to the object of hope.
(145004) Create an environment that
facilitates the patient's practice of her religion, when possible.
(145005) To avoid or conceal the truth.
(5270) Emotional support
Definition: "Providing reassurance,
acceptance, and encouragement in time of stress" (Butcher et al., 2019, p.
74).
Domain
3: Behavioral
Class
R: Coping assistance
(527001) Explore with the patient what
triggered the emotions.
(527002) Support the use of appropriate
coping mechanisms.
(527003) Encourage talking or crying as
a means of decreasing emotional response.
(527004) Staying with the patient and
providing feelings of security during periods of heightened anxiety.
(527005) Refer to counseling services,
if needed.
Finally, it was observed that the
functional patterns that were initially altered: health perception-management,
nutritional-metabolic, elimination, activity and exercise, rest and sleep,
cognitive-perceptual, role-relationships and sexuality-reproduction, have
improved within 24 hours and the 11-week pregnancy is still ongoing, thanks to
the timely and effective application of nursing
interventions.
Execution
In the application of the nursing
interventions and activities, the time for care was organized in three shifts:
6 hours, morning shift; 6 hours, afternoon shift; and 12 hours, night shift. In
addition, the nursing intervention
book (NIC) was used.
|
Table 5. Timeline
of nursing interventions/activities for threatened miscarriage
|
|
Date
|
Interventions/activities
|
|
Shifts
|
|
|
M
|
T
|
N
|
|
Primary
nursing diagnosis
|
|
12/04/2021
|
(6680)
Monitoring of vital signs
|
|
|
|
|
|
Monitor
blood pressure, pulse, temperature, etc and respiratory status, as
appropriate.
|
9
|
6
|
12
|
|
|
Observe
trends and fluctuations in values of the P.A.
|
9
|
6
|
12
|
|
|
Monitor
respiratory rate and rhythm (depth and symmetry).
|
9
|
6
|
12
|
|
|
Monitor
pulse oximetry.
|
9
|
6
|
12
|
|
|
Periodically
monitor skin color, temperature and humidity.
|
9
|
6
|
12
|
|
12/04/2021
|
(4150)
Hemodynamic regulation
|
|
|
|
|
|
Perform
a thorough assessment of hemodynamic status (check blood pressure, heart
rate, pulses, venous pressure).
|
9
|
6
|
12
|
|
|
Recognize
the presence of signs and symptoms early warning signs indicative of the
hemodynamic system.
|
9
|
6
|
12
|
|
|
Determine
the perfusion status (indicate whether the patient is cold, warm or hot).
|
9
|
6
|
12
|
|
|
Place
in Trendelemburg position if necessary necessary.
|
9
|
6
|
12
|
|
12/04/2021
|
(1450)
Nausea management
|
|
|
|
|
|
Encourage
the patient to control her own experience with nausea.
|
9
|
12
|
6
|
|
|
Encourage
eating small amounts of food that is appealing to the person with nausea.
|
9
|
12
|
6
|
|
|
Weigh
the patient regularly.
|
|
|
6
|
|
|
Monitor
the effect of treatment of nausea.
|
9
|
12
|
6
|
|
Risk
of major complication
|
|
12/04/2021
|
(4010)
Hemorrhage prevention
|
|
|
|
|
|
Monitor
the patient closely for signs and symptoms of internal or external bleeding
(example: abdominal swelling).
|
8
|
2
|
10
|
|
|
Maintain
control of intake and consumption elimination.
|
8
|
2
|
10
|
|
|
Maintain
intravenous access.
|
8
|
2
|
10
|
|
|
Maintaining
bed rest during bleeding active.
|
8
|
2
|
10
|
|
|
Instructing
the patient and/or family about the signs and symptoms of hemorrhage.
|
8
|
2
|
10
|
|
12/04/2021
|
(5310)
Giving hope
|
|
|
|
|
|
Help
the patient and family to identify the areas of hope in life.
|
8
|
2
|
10
|
|
|
Encourage
therapeutic relationships with loved ones.
|
|
2
|
|
|
|
Help
the patient design and review goals. related to the object of hope.
|
|
2
|
|
|
|
To
create an environment that facilitates the patient's practice of their
religion, when possible.
|
|
2
|
|
|
|
Avoiding
or disguising the truth.
|
|
2
|
|
|
2/04/2021
|
(5270)
Emotional support
|
|
|
|
|
|
Comment
on the emotional experience with the patient.
|
8
|
2
|
10
|
|
|
Explores
with the patient what has triggered the emotions.
|
8
|
2
|
10
|
|
|
Making
empathic or supportive statements.
|
8
|
2
|
10
|
|
|
Support
the use of defense mechanisms adequate.
|
8
|
2
|
10
|
|
|
Encourage
the patient to express her feelings about the feelings
of anxiety, anger or sadness.
|
8
|
2
|
10
|
|
|
|
|
|
|
Evaluation
A 48-hour follow-up period was
established, observing slight progress (improvement of the ineffective
maternity process and decrease in the risk of bleeding risk) and nursing
activities were evaluated based on the comparison of the patient's initial
health status and the effectiveness of the interventions with respect to the
planned outcomes.
Evaluation
of the main DxE result
|
Table 6. Principal
Diagnosis Main NOC score (Likert Scale: 1-Never demonstrated 2-Rarely
demonstrated. 3-Sometimes demonstrated. 4-Frequently demonstrated. 5-Always
demonstrated.)
|
|
NOC
|
Initial score
|
Target score
|
Score achieved
|
Time
|
|
(1607)
Sanitary conduct prenatal
|
3
|
5
|
5
|
24 hours
|
|
Source:
prepared based on Palomar-Aumatell (2017).
|
|
Table 7. Main
Diagnostic Indicator Scores (Likert Scale: 1-Never demonstrated. 2- Rarely
demonstrated. 3-Sometimes demonstrated. 4-Frequently demonstrated. 5-Always
demonstrated)
|
|
Indicators
|
Initial Score
|
Target score
|
Score Achieved
|
Time
|
|
(160703)
Maintains the visits of prenatal care
|
1
|
5
|
5
|
06 hours
|
|
(160710)
Maintains adequate nutrient intake for gestation.
|
2
|
5
|
5
|
24 hours
|
|
(160723)
Uses supplements of iron
|
1
|
5
|
5
|
24 hours
|
|
(160714)
Prevents exposure to infectious diseases.
|
2
|
5
|
5
|
24 hours
|
|
(160721)
Uses medications according to prescription
|
1
|
5
|
5
|
24 hours
|
|
Source:
own elaboration based on Palomar-Aumatell (2017).
|
Analyzing
the results obtained
As can be seen in table 6, achievement
results are presented about the patient's stability without clinical
manifestations of threatened abortion during the first 24 hours. This risk was
supervised and monitored by executing the nursing activities of the NOC (1607)
Prenatal Health Behavior, as we can observe that the patient obtained a maximum
score of five from the first moment. In order to control and carry out this
development, the following indicators were determined as shown in table 7.
About the indicator (160703), it
maintains the prenatal care visits, since the patient started with an initial
score of one, since in the clinical examination it is found that she did not
receive pre natal control; after the evaluation performed by the gyneco
obstetrician, the obstetrician and the licensed nurse, the intervention reached
a score of five, keeping the patient in a controlled gestational state.
About the indicator (160710), she
maintains an adequate nutrient intake for gestation. Initially, the patient had
a score of two since, in the clinical examination, she indicated preventive NPO
in case the patient would have required a surgical intervention in PCOS. After
the intervention and care, she has been able to achieve a score of five in 24
hours, maintaining stability in her vital functions and vaginal bleeding and
indicating a liquid diet with good oral tolerance.
About indicator (160723), uses iron
supplements; initially, the patient had a score of one, since in the clinical
examination, the patient presented a hemoglobin of 10,5 mg/dl. After
intervention and care, she achieved a score of five at 24 hours. She will
continue treatment with iron to improve her anemia status. This treatment will
continue even after medical discharge, and she will gradually improve regarding
the signs and symptoms of anemia.
About indicator (160714), avoid exposure
to infectious diseases.
Initially, the patient had a score of
two. Because her anemia condition decreased her defenses, she required greater
protection with biosafety measures during non-invasive and invasive procedures.
After the intervention and care, she has reached the maximum score of five, so
she will continue with personal hygiene care and improvement of anemia.
About indicator (160721), she uses medication
as prescribed. Initially the patient had a score of one, considering that in
the clinical evaluation she was admitted as an emergency patient with abdominal
pain and presence of dark discharge via the vagina. After the intervention and
care, she complied with the indicated therapy and, as shown in the nursing
chart and the respective notes, she was administered medications parenterally.
Maintaining a good fluid perfusion with
biosafety measures during the whole process and using sterile material. The
patient scored five, so he will continue with the pharmacological treatment
according to medical indications.
Therefore, the 22-year-old adult patient
who was admitted to the emergency room with abdominal pain and presence of dark
brown vaginal discharge, during her two days of hospital stay and evaluations,
was diagnosed as: 11 weeks pregnant by ultrasound, mild anemia with 10,5mg/dl
of hemoglobin, and currently presents better general condition, afebrile, with
iron medication support and control of vaginal bleeding.
Likewise, she presented an ineffective
maternity process with insufficient prenatal care, inadequate maternal
nutrition, after having received the set of nursing interventions. After two
days of evaluation of functional pattern 9: Sexuality - reproduction, the
patient did not show any dark-colored vaginal bleeding, which determines the
achievement of improving prenatal health behavior through the patient's
actions, in order to promote a good gestation process and a healthy newborn.
Evaluation of the performance of the RCp
The evaluation was performed in relation
to the comparison of the patient's initial health status and the effectiveness
of the resolved actions of the planned
outcomes.
|
Table 8. Evaluation
of the NOC Score of the main CR (Likert Scale: 1. Severe. 2. Substantial 3.
Moderate 4. Level. 5-None)
|
|
NOC
|
Initial Score
|
Target score
|
Score Achieved
|
Time
|
|
(0413)
Blood loss severity
|
4
|
5
|
5
|
48 hours
|
|
Source:
Prepared based on Palomar-Aumatell (2017).
|
|
Table 9. Scoring
of main complication risk indicators
|
|
Indicators
|
Initial score
|
Target score
|
Score achieved
|
Time
|
|
(041307)
Vaginal bleeding
|
4
|
5
|
5
|
24 hours
|
|
(041313)
Pallor of skin and mucous membranes
|
3
|
5
|
5
|
24 hours
|
|
(041306)
Abdominal distention
|
3
|
5
|
5
|
12 hours
|
|
(041316)
Decreased hemoglobin (Hgb)
|
3
|
5
|
4
|
24 hours
|
|
(041317)
Decreased hematocrit (Hto)
|
3
|
5
|
4
|
24 hours
|
|
(041314)
Anxiety
|
4
|
5
|
4
|
24 hours
|
|
(041309)
Decrease in systolic blood pressure
|
4
|
5
|
5
|
6 hours
|
|
(041310)
Pressure reduction diastolic arterial
|
4
|
5
|
5
|
6 hours
|
|
(041312)
Loss of body heat
|
4
|
5
|
5
|
12 hours
|
|
Source:
Elaboration based on Palomar-Aumatell (2017).
|
Interpretation
Table 8 shows that the patient remained
stable without signs of internal or external bleeding. This risk of bleeding
complications has been monitored using the NOC (0413). He also presented the
severity of blood loss, as demonstrated in the permanent monitoring formats.
According to medical indication and nursing activities, it can be demonstrated
that the patient reached a score of five, i.e., in stable condition. In order
to be able to monitor and carry out optimal nursing care, the activities
established in table 9 were applied, with the following indicators:
In relation to indicator (041307)
vaginal bleeding, according to the hourly monitoring record, no signs of
altered vaginal bleeding, both intra-abdominal and extra-vaginal, have been
evidenced. Regarding abdominal swelling and control of vital signs and other
clinical manifestations, a maximum score of five was reached within 24 hours.
Referring to (041313) pallor of skin and
mucous membranes, as an evaluation indicator that in this case manifests the
hemoglobin level through the skin and mucous membranes, the patient has
remained constant and has started treatment with iron supplements to improve
anemia, associated with the improvement of an iron-rich diet, achieving a
maximum score of five at 24 hours.
About (041306) abdominal distension,
this indicator is associated with the risk of intra-abdominal bleeding. During
the patient's evaluation and monitoring, the level of pain was assessed based
on a scale, reaching a score of five in 12 hours.
Regarding the (041316) decrease in
hemoglobin (Hgb), she maintained a hemoglobin of 10,5mg/dl from admission,
which has not changed during her hospitalization period, as shown by the
hemoglobin control. Likewise, the patient was kept in a stable condition with a
final score of four at 24 hours.
The (041317) decrease in hematocrit (Ht)
is closely related to hemoglobin levels since it corresponds to 1/3 of the
total. In this case, it was not altered during the critical period of his stay;
it reached a maximum score of four at 24 hours.
Regarding (041314) anxiety, the patient
initially showed signs of this disorder, associated with her concern about the
current conditions of her pregnancy. After receiving the information from the
physician and the respective emotional support, she regained her
self-confidence. According to the laboratory and ultrasound examination
results, she was allowed the usual help and counseling provided to the patient.
As a result, she achieved a maximum score of four at 24 hours.
Regarding the (041309) decrease in
systolic blood pressure, she has maintained normal blood pressure levels during
her stay. Her decrease would automatically orient to a decrease in blood
volume. In this case, the patient has manifested stability in her vital
functions. She obtained a maximum score of five at 06 hours.
The (041310) decrease in diastolic blood
pressure is related to unexpected changes in blood pressure values, in this
case due to the risk of suffering a bleeding episode at any time. The patient
reached a maximum score of five at 06 hours, maintaining her blood pressure
stable during her hospital stay.
Finally, the (041312) loss of body heat
is associated with a decrease in blood volume and alteration of her vital
functions. According to continuous follow-up and monitoring, the patient has
maintained a normal temperature, and no signs of feeling cold have been
evidenced. Despite this, she achieved a maximum score of five at 12 hours,
i.e., she is in a favorable and stable condition.
After the nursing care provided to the
patient, in which the risk of hemorrhage was the main objective in avoiding
and/or controlling it, constant evaluations of the indicators of the activities
were carried out, so that a term of 6 to 48 hours was achieved to have
significantly decreased the risk of vaginal bleeding; therefore, the patient
presented an initial score of four, and reached the maximum score of five,
which means a regular or stable condition.
It was concluded that bleeding states
during pregnancy are one of the main obstetric complications in prepartum.
According to NANDA I. (2018-2020), the presence of vaginal bleeding, frequency
and amount of bleeding, associated with other manifestations in the vital signs
and skin. Bleeding in pregnant women can be catastrophic, not always being
evident as hemoperitoneum or hematomas. Therefore, blood pressure and pulse
should be checked regularly for any patient suspected of hypovolemic shock.
In the professional nursing practice,
meaning has been given to the reality where care is performed, applying the
systematic method to organize, execute, and evaluate the required nursing
interventions. This is the case of Jean Watson's "Theory of human
care" and Callista Roy's "Adaptation Model", which are
consistent with applying the care plan and nursing activities, denoting
professional commitment and responsibility. This procedure is scientific, since
it involves planning, organization, control, monitoring, and evaluation of the
quality of nursing care in daily care based on health guidelines, the
availability of resources, and the use of technology in care management. Thus,
the care provided to the patient allowed for attentive listening, dialogue, and
respect for her rights during care and spiritual assistance.
On the other hand, the patient's
hemodynamic support was achieved without any signs of hemorrhage. This risk of
complication has been permanently monitored according to medical indication and
the NOC indicator (0413) severity of blood loss. Thus, a final score of five
was achieved, i.e., she is in a state of normalcy.
Based on the above, it is confirmed that
the planned results for the patient's nursing care have been achieved with the
application of the activities in the established time, achieving favorable
results. In addition, the intervention has been timely in the health care
process was ineffective, as evidenced by the maximum rating of five points
achieved in 48 hours. In conclusion, the nursing care plan was successful,
reflected in the patient's improvement and absence of complications.
DISCUSSION
The patient in the present study was
admitted to the gynecology department after being seen in the emergency
department. She presented with threatened miscarriage at 11 weeks of gestation
and CR of hemorrhage, considering her clinical condition as high risk for her
health. Likewise, after the respective literature review, numerous studies have
been obtained that show the fundamental role of nursing in comprehensive and
quality care, in order to help patients with threatened abortion
(Carvajal-Cabrera & Barriga-Cosmelli, 2021).
This involves making a care plan
corresponding to the use of the fundamental nursing tool (PAE), which confers
autonomy in collecting information from the patient and in executing a series
of activities that reinforce the weaknesses or discomforts at different levels:
physical, emotional, spiritual, and social. In this sense, assistance is
emphasized in the most relevant aspects that nursing can address
(Franco-Campos, 2019).
It should be noted that the care plan
makes it possible to protocolize nursing actions about the needs of the patient
with threatened miscarriage, for monitoring, evaluation, and consolidation, as
an axis for improving interventions in patients with similar diagnoses.
Therefore, every pregnant woman in her first trimester experiences mixed
feelings between illusion and fear of miscarriage until after 20 weeks.
Pregnant patients are emotionally labile and need good support and treatment.
The patient's health care team is a
human team that makes them feel that they are valuable and that they have a
team of health care professionals attentive to their hospital stay and the
resolution of their health problem.
It is also emphasized that, in this care
process, it was important for the participation of the family and the couple
through their support, the resolution of doubts, and the expansion of
information about the patient; this allowed covering all the components of the
holistic care provided in the nursing intervention. By integrating the close
members of the pregnant woman, they became indirect participants in improving
the patient, avoiding complications, and decreasing the hospital stay (Macias
et al., 2018).
In nursing interventions, two theories
have been applied in terms of the care plan: Jean Watson's "Humanized Care
Theory" (which focuses on the patient's priority needs and refers to
holistic and humane care) and Callista Roy's "Adaptation Theory,"
which takes into consideration the assessment of behavior and stimuli that may
influence the adaptation of the woman in a situation of threatened abortion.
The relationship between the theories
and the patient's situation is observed after the diagnosis of threatened
miscarriage, which usually occurs in the first 20 weeks of pregnancy (i.e., in
the first trimester), with the possibility of improvement with effective
treatment in most cases. However, proper care and self-care are required to
improve their lifestyle.
On the other hand, the process of
ineffective motherhood occurs as a consequence of the inability to prepare for
and/or maintain a healthy pregnancy, and it is here where the nursing
professional plays an important role in the management of the prevention of
bleeding complications, with strict and scientific compliance with
pharmacological and non-pharmacological treatment.
The CR of hemorrhage could occur if the
patient has any risk factors that could hinder gestation. In this sense,
nursing actions play an essential role as they are aimed at prevention and
timely intervention to prevent this problem from worsening; in addition, it is
helpful to apply interventional procedures and techniques to restore health
with an intersubjective attitude, with the support of technology and promoting
a relationship between the caregiver and the patient.
All of the above agrees with
Guerrero-Hernandez et al. (2017) and Carvajal-Cabrera and Barriga-Cosmelli
(2021) consider threatened miscarriage a state that could end in miscarriage
before 20 weeks of pregnancy, and in most cases vaginal bleeding stops on its
own and the pregnancy continues its course; however, other times the threat
progresses to miscarriage: at least 20-30 % of pregnant women have hemorrhage
in the first trimester, and in known pregnancies, the average miscarriage is
approximately 10 %, usually presenting between seven and 12 weeks of gestation
(Reproductive, 2018). Also, hemorrhage is one of the first causes of maternal
perinatal morbidity and mortality, making immediate, timely, and effective care
essential in order to avoid subsequent complications that cause family pain.
In conclusion, health professionals are
committed to carrying out a broad and thorough nursing assessment to prevent
any risk of complications from aggravating the patient's already existing
situations. The study shows that, after having provided care to the patient, a
favorable evolution was evidenced compared to the initial phase of the care
plan.
Limitations
The limitations encountered throughout the study's
development have been: Limited time to follow up on the case under study, since
the severity of the situation in which the patient found herself and the
consequences it entails require more time for the improvement that has been
obtained after the actions carried out. Therefore, a long-term nursing care
plan will be continued.
Also, the period was restricted for
follow-up of the threatened abortion case under study. Social isolation due to
the COVID-19 pandemic has limited the time for family visits in the hospital.
In addition, the limited conditions for access to information by the patient's
family played a restrictive role, since no visits were permitted due to the
pandemic, nor were additional data considered very intimate because they were
part of the professional secret.
CONCLUSIONS
The role of the nurse is an important
place in the care of patients who are attended to in the obstetrics and
gynecology service; among the different cases, there is the threat of abortion.
This implies that the nursing professional must strengthen his/her competencies
for the timely and assertive management of these cases, avoiding complications
and favoring the well-being and health of the patients.
Likewise, the importance of knowing in
depth the pathological process of the health problems presented by the patients
attended to daily in the hospital environment is highlighted. An effective
nurse diagnostician establishes the necessary clinical judgments to know the
pathophysiology and behavior of the diseases of the service where he/she works
in order to make a good diagnosis.
On the other hand, one of the leading
causes of maternal morbidity and mortality in Peru is puerperal hemorrhage,
which requires that nursing professionals in the area of obstetrics and
gynecology know the preventive measures and premonitory signs of hemorrhage in
order to control and reverse the cases, avoiding major complications. Also, it
is of vital importance that prenatal care education occurs in prenatal
controls, in order to favor the gestation process and the conception of the
fetus, avoiding risks in the maternity process.
In conclusion, the nursing professional
must know and adequately manage the nursing care process, which is an
indispensable tool in managing maternal care. Maintaining a standardized
language through the interrelation of NANDA I, NOC, NIC, and Linda Juall
Carpenito's collaborative problems will result in optimal and focused attention
to the problems and risks that may arise in obstetric events, such as
threatened abortion.
BIBLIOGRAPHIC REFERENCES
1. Abanto Arana, C. F., &
Anhuamán Morillo, L. A. (2019). Conocimientos, prácticas maternas y frecuencia
de infecciones respiratorias agudas en niños menores de cinco años. [Tesis de
Licenciatura] [Universidad Nacional de Trujillo]. https://dspace.unitru.edu.pe/bitstream/handle/UNITRU/11623/1849.pdf?sequence=3&isAllowed=y
2. Alayo Cuzcano, C. G., Castañeda
Alfaro, I. I., & Tarrillo Valcazar, C. M. (2018). Conocimientos y practicas
de la enfermera sobre la valoración del paciente con sedación mecánica en la
Unidad de Cuidados Intensivos Pediátricos. [Tesis de Especialidad] [Universidad
Peruana Cayetano Heredia]. https://repositorio.upch.edu.pe/bitstream/handle/20.500.12866/4581/Conocimientos_AlayoCuzcano_Cristina.pdf?sequence=1&isAllowed=y
3. Alayo Huatay, H. K. (2019).
Efecto del programa: ‘“cuidando mi salud”’ en el nivel de información y
ansiedad en gestantes programadas para cesárea. [Tesis de Segunda Especialidad]
[Universidad Nacional de Trujillo]. https://dspace.unitru.edu.pe/bitstream/handle/UNITRU/14920/2E603.pdf?sequence=1&isAllowed=y
4. Álvarez Maita, R. A. (2020).
Percepción del familiar sobre comunicación asertiva y apoyo emocional que
brinda el profesional de Enfermería en la Unidad de Cuidados Intensivos de un
hospital pediátrico de Lima, 2020. [Tesis de Especialidad] [Universidad Peruana
Unión].
https://repositorio.upeu.edu.pe/bitstream/handle/20.500.12840/3511/Rocio_Trabajo_Especi
alidad_2020.pdf?sequence=1&isAllowed=yANAEL. (2015). El aborto: métodos y
consecuencias. Centro Gnóstico ANAEL. https://anael.org/es/aborto
5. Bergallo, P., Jaramillo Sierra,
I. C., & Vaggione, J. M. (2018). El Aborto en América Latina: Estrategias
jurídicas para luchar por su legalización y enfrentar las resistencias
conservadoras. (Siglo XXI (ed.); 1ra ed.). Grupo Editorial Siglo Veintiuno XXI.
https://www.cmi.no/publications/file/6584-movimiento-transnacional-contra-el-derecho-
al.pdf
6. Bruno Maldonado, Z. E. (2019).
Proceso de atención de enfermería a paciente post operada de cesárea por oligo-
hidramnios y cesárea anterior del Servicio de Gineco-Obstetricia de un hospital
de Huaral, 2018. [Tesis de Segunda Especialidad] [Universidad Peruana Unión]. https://repositorio.upeu.edu.pe/bitstream/handle/20.500.12840/1955/Zulmy_Trabajo_Academico_2019.pdf?sequence=1&isAllowed=y
7. Bunce, E. E., & Heine, R. P.
(2020). Edema en los miembros inferiores en la
segunda mitad del embarazo - Ginecología y obstetricia - Manual MSD versión
para profesionales. Manual MSD: Versión Para Profesionales. https://www.msdmanuals.com/es-pe/professional/ginecología-y-obstetricia/síntomas-durante-el-embarazo/edema-en-los-miembros-inferiores-en-la-segunda-mitad-del-embarazo
8. Butcher, H., Bulecheck, G., Dochterman,
J. M., & Wagner, C. (2018). Clasificación de
Intervenciones de Enfermería (NIC) (Elsevier (ed.); 7th ed.). Elsevier.
https://www.elsevier.com/books/clasificacion-de-intervenciones-de-enfermeria-
nic/butcher/978-84-9113-404-6
9. Butcher, H. K., Bulechek, G. M.,
Dochterman, J. M., & Wagner, C. (2019). Clasificación
de Intervenciones de Enfermería (NIC) (7th Editio). Elsevier. https://cercabib.ub.edu/iii/encore/record/CRb2693537SGIGA361301P0,7OrightresultUX1?lang=cat
10. Carbajal Sánchez, R. E., &
Nery Segura, M. M. (2018). Salud mental y calidad de vida en el trabajo del
personal de la central de esterilización del hospital “Julio César Demarini
Caro”, Chanchamayo - 2017. [Tesis de Maestría] [Universidad Norbert Wiener]. http://repositorio.uwiener.edu.pe/bitstream/handle/123456789/2867/TESISCarbajalRosa-NeryMaría.pdf?sequence=1&isAllowed=y
11. Carvajal Cabrera, J. A., &
Barriga Cosmelli, M. I. (2021). Manual de Obstetricia y Ginecología (Pontificia
Universidad Católica de Chile - Escuela de Medicina - Facultad de Medicina
(ed.); 12th ed.). https://medicina.uc.cl/publicacion/manual-obstetricia-y-ginecologia/
12. Cornejo Sánchez, L. L. (2020).
Percepción del paciente sobre Cuidado Humanizado a la luz de Watson - Servicio
de Cirugía H.R.D. “Las Mercedes”, Chiclayo - 2019. [Tesis de Licenciatura]
[Universidad Señor de Sipán]. https://repositorio.uss.edu.pe/bitstream/handle/20.500.12802/6536/CornejoSánchezLeslieLucía.pdf?sequence=1&isAllowed=y
13. Diaz Rivera, V. G. (2017).
Percepción del familiar respecto al cuidado humanizado que brinda la enfermera
al paciente en la UCI - UCIN del Hospital Nacional Arzobispo Loayza, Lima -
2017. [Tesis de Especialidad] [Universidad Nacional Mayor de San Marcos]. http://cybertesis.unmsm.edu.pe/bitstream/handle/20.500.12672/7102/Diaz_rv.pdf?sequence=1&isAllowed=y
14. Dulay, A. (2020, October).
Preeclampsia y eclampsia. Manual MSD Versión Para Profesionales. https://www.msdmanuals.com/es-pe/professional/ginecología-y-obstetricia/anomalías-del-embarazo/preeclampsia-y-eclampsia
15. EAFIT. (2018). El cuidado y el
mutuo cuidado. https://www.eafit.edu.co/bienestar-
universitario/acerca-de-la-direccion/Documents/cuidado-mutuo-cuidado.pdf
16. eCIE10ES. (2022, January).
eCIE-Maps - CIE-10-ES Diagnósticos. Edición Electrónica de La CIE-10-ES
Diagnósticos. https://eciemaps.mscbs.gob.es/ecieMaps/browser/index_10_mc.html
17. Franco Campos, H. L. (2019).
Proceso de atención de enfermería aplicado a paciente post operada de cesárea
por expulsivo prolongado y macrosomía fetal del Servicio de Gineco Obstetricia
de un hospital de Huacho, 2018. [Tesis de Segunda Especialidad] [Universidad
Peruana Unión]. https://repositorio.upeu.edu.pe/bitstream/handle/20.500.12840/2087/Haydee_Trabajo_Academico_2019.pdf?sequence=1&isAllowed=y
18. Frederico, M., Arnaldo, C., Decat,
P., Juga, A., Kemigisha, E., Degomme, O., & Michielsen, K. (2020). Induced
abortion: a cross-sectional study on knowledge of and attitudes toward the new
abortion law in Maputo and Quelimane cities, Mozambique. BMC Women’s Health
2020 20:1, 20(1), 1–13. https://doi.org/10.1186/S12905-020-00988-6
19. Fuertes Moreno, A. I. (2019). Factores
clínicos y sociodemográficos asociados a preeclampsia en gestantes atendidas en
el servicio de emergencia del periodo enero-julio del Hospital de Apoyo II
Sullana, 2018. [Universidad Privada Antenor Orrego]. http://repositorio.upao.edu.pe/bitstream/upaorep/5319/1/REP_MED.HUMA_ISABEL.FUE
RTES_FACTORES.CLÍNICOS.SOCIODEMOGRÁFICOS.ASOCIADOS.PREECLAMPSIA.GESTANTES.ATENDIDAS.SERVICIO.EMERGENCIA.PERIODO.ENEROJULIO.HOSPITAL.APOYO.II.SULLANA.2018.pdf
20. Gaspar Huánuco, S. L., &
Torres Rojas, A. M. (2018). Factores que influyen en las mujeres de edad fértil
en la decisión para provocarse un aborto del Servicio Gineco Obstetricia del
Hospital Regional Docente Materno Infantil El Carmen, periodo Junio - Agosto
del 2017. [Tesis de Titulción] [Universidad Privada de Huancayo Franklin
Roosevelt]. https://repositorio.uroosevelt.edu.pe/bitstream/handle/ROOSEVELT/103/TesisAborto.pdf?sequence=1&isAllowed=y
21. González Aguña, A., &
Santamaría García, J. M. (2015). El ciclo del cuidado: el modelo profesional de
cuidado desde el enfoque del pensamiento. Ene, 9(1), 0–0. https://doi.org/10.4321/s1988-348x2015000100003
22. Guerrero Hernandez, L., Huamán
Sialer, C., & Manrique Rosas, C. (2017). Carga laboral y actitud del
profesional de enfermería hacia el familiar del paciente hospitalizado en la
Unidad de Cuidados Intensivos Adultos de una clínica privada. [Tesis de
Especialidad] [Universidad Peruana Cayetano Heredia]. https://repositorio.upch.edu.pe/bitstream/handle/20.500.12866/718/Carga_GuerreroHernandez_Leidy.pdf?sequence=1&isAllowed=y
23. Herdman, H., & Shigemi, K.
(2019). Diagnósticos enfermeros definición y clasificación 2018- 2020. In
ELSEVIER. Elsevier España. https://www.elsevier.com/books/diagnosticos-enfermeros-definiciones-y-clasificacion-2018-2020-edicion-
hispanoamericana/herdman/978-84-9113-450-3
24. Herdman, T. H., & Kamitsuru, S.
(2017). Diagnósticos Enfermeros: Definiciones y
Casificación.
25. NANDA Internacional. https://s67d378623b10162d.jimcontent.com/download/version/1479845861/module/898643
8569/name/NANDA2015-201717.pdf
26. Huanca Morales, M. P. (2020).
Pielonefritis aguda y embarazo en Hospital II-1 MINSA - 2018. [Tesis de Segunda
Especialidad] [Universidad José Carlos Mariátegui]. http://repositorio.ujcm.edu.pe/bitstream/handle/20.500.12819/985/Milagros_trab-acad_titulo_2020.pdf?sequence=1&isAllowed=y
27. INEI. (2019, December 31).
ENDES realizadas. Instituto Nacional de Estadística e Informática PERÚ. https://proyectos.inei.gob.pe/endes/
28. Johnson, M., Bulechek, G., Butcher,
H., McCloskey Dochterman, J., Maas, M., Moorhead, S., & Swanson, E. (2007).
Interrelaciones
NANDA, NOC y NIC: Diagnósticos enfermeros, resultados e intervenciones. http://www.untumbes.edu.pe/vcs/biblioteca/document/varioslibros/0880.
Interrelaciones.
29. Nanda%2C Noc y Nic.
Diagnósticos enfermeros%2C resultados e intervenciones.pdf
30. león, W., Yépez, E., Nieto, M.
B., Grijalva, S., Cárdenas, M., Carrión, F., & Miranda, O. (2016).
31. Conocimientos, actitudes y
prácticas sobre aborto en una muestra de médicos gineco- obstetras de Ecuador.
Revista Peruana de Ginecología y Obstetricia, 62(2). http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S2304-51322016000200004
32. Llanos Cerquín, J. (2018).
Factores de riesgo sociales que influyen en las consecuencias psicológicas post
aborto Hospital Regional Docente Cajamarca 2016. [Tesis de Titulación]
[Universidad nacional de Cajamarca]. https://repositorio.unc.edu.pe/bitstream/handle/UNC/1792/FACTORESDESOCIALESQUEINFLUYENENLASCONSECUENCIASPSICOLÓGICASPOSTABORTOHOSPITALR.pdf?sequence=1&isAllowed=y
33. Martínez Montaño, M. del L.
(2021). El informe final de la investigación: Metodología de la investigación
para el área de la salud (AccessMedicina (ed.); 2da ed.). McGraw
Hill Medical. https://accessmedicina.mhmedical.com/content.aspx?bookid=2448§ionid=193961606
MINSA-CSS. (2015). Guías de Manejo de las
Complicaciones en el Embarazo (Programa 34. Nacional de Salud Sexual y
Reproductiva Programa Materno Infantil). https://data.miraquetemiro.org/sites/default/files/documentos/guias-complicaciones-
embarazo_diciembre_2015.pdf
34. MINSA. (2018, September 14).
Minsa: el embarazo adolescente incrementa el riesgo de mortalidad materna y del
niño por nacer | Gobierno del Perú. Ministerio de Salud - Perú. https://www.gob.pe/institucion/minsa/noticias/19292-minsa-el-embarazo-adolescente-incrementa-el-riesgo-de-mortalidad-materna-y-del-nino-por-nacer
35. Moorhead, S., Swanson, E., Jphnson,
M., & Maas, M. L. (2019). Clasificación de
resultados de enfermería (NOC) :
medición de resultados en salud. (6th ed.). Elsevier.
36. NANDA diagnósticos enfermeros:
definiciones y clasificación 2018-2020. (2019). In Biblioteca San Juan de Dios
(11th ed.). Elsevier España S.L.U. https://bibliosjd.org/2019/11/04/nanda-2018-2020-nueva-edicion/#.X6MXzGhKjcc
37. NANDA Internacional. (2018). La
Cuidadología es la ciencia del cuidado. NANDA 2018-2020 - El Diagnóstico
Enfermero. http://www.eldiagnosticoenfermero.es/2017/08/nanda-2018-
2020.html
38. Neglia Cermeño, M. E. (2017).
Cuidados de enfermería en el post operatorio inmediato a pacientes cesareadas
del Hospital II EsSalud Huaraz - Ancash, 2014 - 2017. [Tesis de Segunda
Especialidad] [Universidad Nacional del Callao]. http://repositorio.unac.edu.pe/bitstream/handle/20.500.12952/4916/negliacermeñoenfermeria2017.pdf?sequence=1&isAllowed=y
39. Neyra Díaz, A. del P., &
Palominpo Bonifacio, E. N. (2019). Factores de riesgo para la depresión
postaprto en madres adolescentes atendidas en el Hospital María Auxiliadora,
2017. [Tesis de Licenciatura]. http://repositorio.uwiener.edu.pe/xmlui/bitstream/handle/123456789/3153/TESIS/PalominoEvelyn-NeyraAdela.pdf?sequence=1&isAllowed=y
40. Ochoa Marieta, C., Reus, R.,
& Rogel Cayetano, S. (2018). Amenaza de aborto: causas, síntomas y
tratamiento. Reproducción Asistida ORG. https://www.reproduccionasistida.org/amenaza-
de-aborto/
41. Ocón Cabria, A. M. (2017). El
aborto: aspectos filosóficos, éticos y jurídicos. [Tesis Doctoral] [Universidad
Complutense de Madrid]. https://eprints.ucm.es/id/eprint/43243/1/T38908.pdf
42. OMS. (2019, October 25). Un
nuevo estudio de la OMS relaciona las altas tasas de embarazos no planificados
con las deficiencias de los servicios de planificación familiar. Organización
Mundial de La Salud. https://www.who.int/es/news/item/25-10-2019-high-rates-of-unintended-pregnancies-linked-to-gaps-in-family-planning-services-new-who-study
43. OMS. (2020, April). La OMS y
sus asociados hacen un llamamiento urgente para que se invierta en el personal
de enfermería. Organización Mundial de La Salud. https://www.who.int/es/news/item/07-04-2020-who-and-partners-call-for-urgent-investment-in-nurses
44. Personal de Mayo Clinic.
(2020). Aborto espontáneo - Síntomas y causas. Mayo Clinic. https://www.mayoclinic.org/es-es/diseases-conditions/pregnancy-loss-
miscarriage/symptoms-causes/syc-20354298
45. Pesut, D. J., & Herman, J.
(2019). Razonamiento clínico: el arte y la
ciencia del pensamiento crítico y creativo.
46. Pezantes Lazo, E. J. (2018).
Proceso de atención de enfermería aplicado a paciente poscesareada por
preeclampsia severa de la Unidad de Recuperación Posanestésica de un hospital
de Lima, 2018. [Tesis de Especialidad] [Universidad Peruana Unión]. https://repositorio.upeu.edu.pe/bitstream/handle/20.500.12840/1421/Elizabeth_Trabajo_Académico_2018.pdf?sequence=5&isAllowed=y
47. Ramos, S., & Fernández
Vázquez, S. S. (2020). ¿Porqué abortan las mujeres?: Contexto y biografía en
las experiencias de aborto. REDAAS - Red de Acceso Al Aborto Seguro, 12. www.cedes.org
48. Ríos Canales, C. I., Vera
Véliz, R. C., & Mantilla Cruzado, V. (2018). Aborto en adolescentes
atendido en el Hospital I. Florencia de Mora. EsSalud. Enero 2016 – Diciembre
2017.
49. Revista Médica de Trujillo,
13(3). https://revistas.unitru.edu.pe/index.php/RMT/article/view/2097
50. Rivero Navia, M. J., &
Pintado Abad, S. V. (2017). Frecuencia y factores de riesgo de aborto en
mujeres de 20 a 40 años en el Hospital Mariana de Jesús durante el periodo de
enero y febrero del 2017. [Tesis de Titulación] [Universidad Católica de Santiago
de Guayaquil]. http://repositorio.ucsg.edu.ec/handle/3317/8043
51. UNFRA-Perú. (17 de Mayo de
2021). Conmemoramos la Semana de la Maternidad Saludable, Segura y Voluntaria.
LIma, Lima, Perú.
52. Vásquez De La Torre, A. K.
(2018). Actitudes hacia el aborto en adolescentes de dos instituciones
educativas. [Tesis de Licenciatura] [Universidad Señor De Sipán]. https://repositorio.uss.edu.pe/bitstream/handle/20.500.12802/7038/VásquezDeLaTorreAshleyKatheryne.pdf?sequence=1&isAllowed=y
FINANCING
There is no funding for this work.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Marcela F. Monzón-Murillo, Sofía D. Vivanco-Hilario,
Wilter C. Morales-García.
Research: Marcela F. Monzón-Murillo, Sofía D. Vivanco-Hilario,
Wilter C. Morales-García.
Methodology: Marcela F. Monzón-Murillo, Sofía D. Vivanco-Hilario,
Wilter C. Morales-García.
Project administration: Marcela F. Monzón-Murillo, Sofía D. Vivanco-Hilario,
Wilter C. Morales-García.
Original drafting and editing: Marcela F. Monzón-Murillo, Sofía D. Vivanco-Hilario,
Wilter C. Morales-García.
Writing-revision and editing: Marcela F. Monzón-Murillo, Sofía D. Vivanco-Hilario,
Wilter C. Morales-García.
ANNEXES
Appendix
A. Plan of care
AFFILIATION
DATA
User's
name: Address:
HOSPITALIZATION
DATA
HCL:
Account: Insurance: Origin: Outpatient (
) Emergency ( ) SOP ( ) Referred
Age:
Religion:
from:
Grade
of education: Occupation: Source of
Information: Patient ( ) Relative/friend ( ) Other:
Method
of arrival: Walking ( ) Stretcher ( ) Wheelchair ( ) Reason for admission:
Dx.
Medical: Date of assessment:
ASSESSMENT
ACCORDING TO FUNCTIONAL PATTERNS OF HEALTH
FUNCTIONAL
PATTERN OF HEALTH PERCEPTION/CONTROL
History
of disease and surgical history:
HTA
( ) DM ( ) Miscarriages ( ) Gastritis/ulcer ( ) TB ( ) Asthma ( ) HIV (
) VDRL ( ) Other
Surgeries:
No ( ) Yes ( )
Allergies
and other reactions:
Pharmaceuticals:
Food: Signs-symptoms: Others Risk
factors:
Consumption:
Tobacco No ( ) Yes( ) Alcohol No( ) Yes( ) Drugs No( ) Yes( ) Yes ( )
Medications
(with or without medical indication)
What
are you currently taking? Dose/Freq. Last dose
Hygiene
condition: Good ( ) Fair ( ) Poor ( ) Poor ( )
What
do you know about your disease current?
Where
do you go when you get sick?
What
do you need to know about your disease?
FUNCTIONAL
PATTERN OF SEXUALITY/REPRODUCTION
Obstetric
Formula: G P EG: CPN NO.: FUR: FPP:
Breasts:
sensitive ( ) Not sensitive( ) soft( ) hard( ) secretory( )
(
) nonsecretory ( ) hard mass ( ) abscess ( ) healing ( ) bandage ( ) Nipples:
Formed ( ) flat ( ) inverted ( ) inverted ( ) cracked ( ) Uterus: Gravid ( )
not gravid ( ) contracted ( ) not contracted( ) Uterine height:
Uterine
dynamics:
Freq:
Tone: Intensity: Genitalia: normal ( )
edema ( ) hematoma ( ) other:
Vaginal
discharge: white ( ) yellow( ) yellow( ) green( ) green( ) foul-smelling ( )
Volume vaginal bleeding:
M:
T: N:
Vaginal
plug: Yes ( ) No ( ) No ( ) No. of gauze: Amniotic fluid
leakage: qty:
color:
odor:
Lochia:
cant: color: odor: Fetal
Movements: Yes ( ) No ( )
FCL:
Observation:
NUTRITIONAL-METABOLIC
FUNCTIONAL PATTERN
Weight:
Height: BMI: T: °C
Wound:
Location and description:
Glucose:
Hb:
Protected
with dressing: clean ( ) dry ( ) stained ( ) wet ( ) without signs of phlogosis
( ) with signs of phlogosis ( ) with ecchymotic borders ( ) ecchymotic ( )
With
drain: tubular ( ) laminar( )Infected: No( ) Yes( )
FUNCTIONAL
PATTERN OF RELATIONSHIPS
ROLE
Occupation:
Marital Status: Single ( ) Married( ) Cohabitant( ) Divorced( )
With
whom do you live? Alone ( ) With your family ( ) Other
Sources
of support: Family ( ) Friends ( ) Others
Family
conflict/violence: Yes ( ) No ( )
Attempted/suicide
Yes ( ) No ( ) When:
AGA:
Skin
and mucosa: pinkish ( ) pale ( ) cyanotic ( ) ikteric ( ) warm ( ) warm ( )
cold ( ) hydrated ( ) dehydrated ( ) dry ( ) turgid ( ) edematous ( )
hemorrhagic ( ) crampy ( ) diaphoresis ( ) over hydration ( )
Thirst
( ) Sweating ( ) Integrity: Intact ( ) Lesions ( ) Observation:
Nutrition:
Fluid intake: 24 hr / food: 24 hr Route of administration: oral ( ) enteral(
) SNG( ) SNG( ) ostomy( ) parenteral( ) peripheral ( )
Appetite:
Norm l( ) Decreased( ) Increased( ) Type of diet:
Oral
cavity: Denture: Complete ( ) Incomplete ( ) Denture ( )
Prosthesis( ) Difficulty swallowing: Yes ( ) No ( ) Nausea ( ) Pyrosis ( )
Vomiting ( )
Oral
hygiene status: Poor ( ) Fair ( ) Good ( ) Good ( ) Weight change during the
last days: Yes ( ) No( )
FUNCTIONAL
PATTERN OF ACTIVITY - EXERCISE
age:
( ) Underweight:( ) Specify:
RESPIRATORY
ACTIVITY FR:
Breathing:
superficial
l( ) deep( ) Dyspnea: At rest( )
On
exercise( ) Tires easily: No ( ) Yes( )
Cough:
dry( ) productive( ) expectoration:
Cough
reflex: Present ( ) Absent ( ) Absent ( ) Diminished ( )
Secretions:
No( ) Yes ( ) Characteristics:
Soft
( ) depressible ( ) distended ( ) tympanic ( ) globular ( ) painful ( )
Emotional
state Calm ( ) Anxious ( ) Negative ( ) Fearful ( ) Irritable ( ) Different
( ) Depressed ( )
Main
concerns/comments:
O2:
No ( ) Yes ( ) Mode: l/min
FUNCTIONAL
ELIMINATION PATTERN
Bowel
habits No. of bowel movements/day:
Normal
(CIRCULATORY ACTIVITY) Constipation ( ) Diarrhea ( ) Incontinence ( )
Peripheral
pulse:
P/A: unaltered:
Bladder
habits Frequency: / day pollakiuria ( ) Dysuria ( ) nocturia ( ) Proteinuria:
Albumin in urine:
Hypotension
() hypertension () tachycardia ( ) bradycardia ( )
cold
extremities( ) numbness( ) sensitivity of limbs( )
arrhythmias(
) precordial pain( ) pacemaker( )
Edema: No
Yes Location:
Others:
FUNCTIONAL
PATTERN OF REST – SLEEP +( ) ++ ( ) +++( )
Presence
of invasive lines: Peripheral catheter:
EXERCISE:
SELF-CARE CAPACITY
1=
Independent 3= Completely dependent 2= Partially dependent
Additional
comments:
Sleeping
hours:
Sleeping
problems: Yes ( ) No( )
Specify:
Do
you use any medication to sleep? Yes ( ) No ( ) Specify:
FUNCTIONAL
PATTERN OF VALUES - BELIEFS
Religion:
Assistive
devices: none ( ) Wheelchair ( ) Other:
Religious
restrictions:
Request
chaplain's visit: Yes ( ) No ( )
Mobility
of limbs: Preserved ( ) Flaccidity ( ) Contractures ( ) Paralysis ( )
Muscle
strength: Conserved ( ) Decreased ( ) Additional comments:
PERCEPTUAL-COGNITIVE
FUNCTIONAL PATTERN
Oriented:
Time ( ) Space ( ) Person ( ) Disoriented ( ) confused ( ) drowsy ( ) agitated
( ) convulsing ( )
stupor(
) coma( ) lethargic( ) Communicative ( ) not very communicative ( )
GLASGOW
SCALE SCORE:
Hearing:
no impairment ( ) hearing loss ( ) hearing aids ( ) prosthesis ( ) Vision: no
impairment ( ) impaired ( ) blindness ( ) prosthesis ( ) Hallucinations:
auditory ( ) visual ( ) olfactory ( ) tactile ( ) tactile ( ) Alterations of
thought: dementia ( ) Speech/language:
Pain:
No ( ) Yes ( ) Location: Headache ( ) Uterine Dynamics ( )
Pain
Scale: 1 2 3 4 5 6 7 8 9 10 Other:
Additional
comments:
Nurse's
name:
Signature: CEP:
Date: CURRENT MEDICAL TREATMENT:
AUXILIARY
EXAMINATIONS:
TESTS
OF FETAL WELL-BEING:
NST: TST:
ECO Biofco:
Appendix
B: Informed Consent
Universidad
Peruana Unión Graduate School
UPG
Health Sciences Purpose and procedures
I
have been informed that the title of the academic work is "Nursing role in
the care of a patient with threatened abortion in the obstetrics and gynecology
service of a hospital in Lima, 2021". The objective of this study is to
apply the Nursing Care Process to the patient with initials M.R.V. This
academic work is being carried out by Lic. Marcela
Flor Monzón Murillo and Lic. Sofía Dora Vivanco Hilario, under the supervision
of Dr. María Teresa Cabanillas Chávez. The information
provided through the assessment guide, interview and physical examination will
be confidential and will be used only for the purposes of the study.
Risks
of the study
I
have been informed that there is no physical, chemical, biological, and
psychological risk associated with this research. However, since some personal
information will be obtained, there is a possibility that my identity may be
discovered from the information given. However, precautions such as
identification by numbers will be taken to minimize such a possibility.
Benefits
of the study
There
is no monetary compensation for participation in this study.
Voluntary
participation
I
have been informed that my participation in the study is completely voluntary
and that I have the right to withdraw my consent at any point before the report
is finalized, without penalty. The same applies for my initial refusal to
participate in this project.
Having
carefully read the consent form and listened to the oral explanations of the
investigator, I voluntarily sign the present document.
Name
and surname: M.R.V. DNI: 00000000
Date:
January 28, 2022
Signature
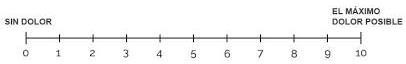
Figure C 1. Visual
Analog Scale (VAS) for pain measurement
|
Bed
mobilization
|
|
Wander
|
|
Toileting/bathing
|
|
Food intake
|
|
Dress
|
Appendix
C. Rating scales used
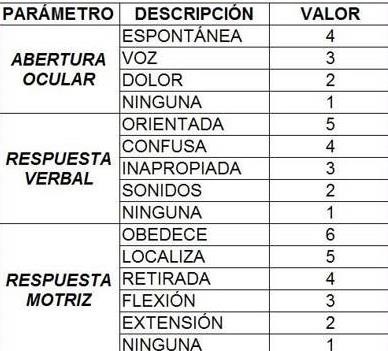
Figure C 2. Glasgow
BMI rating scale

Figure
C 3.
Glasgow BMI rating scale
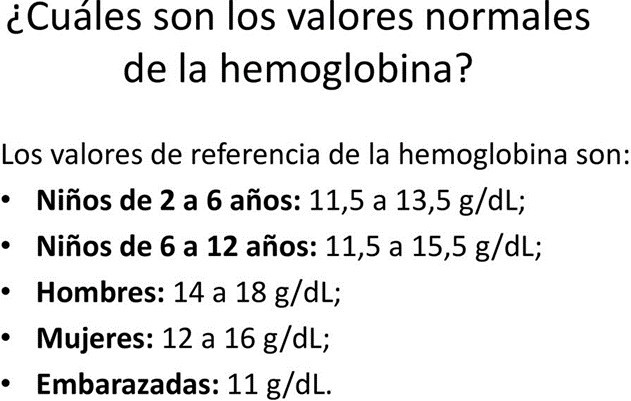
Figure C 4. Hemoglobin
reference values
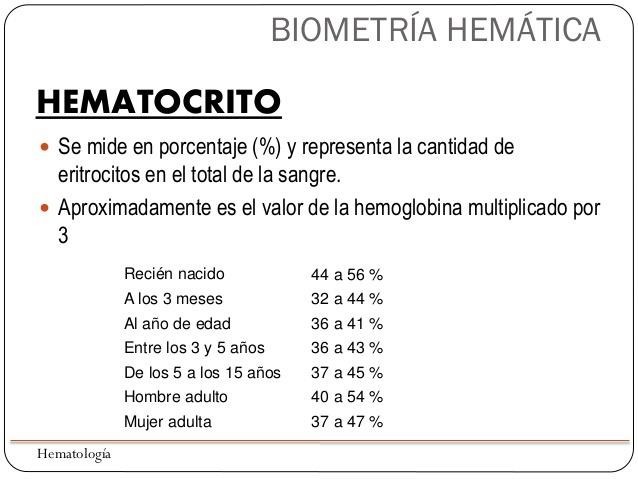
Figure C 5. Anemia
rating scale
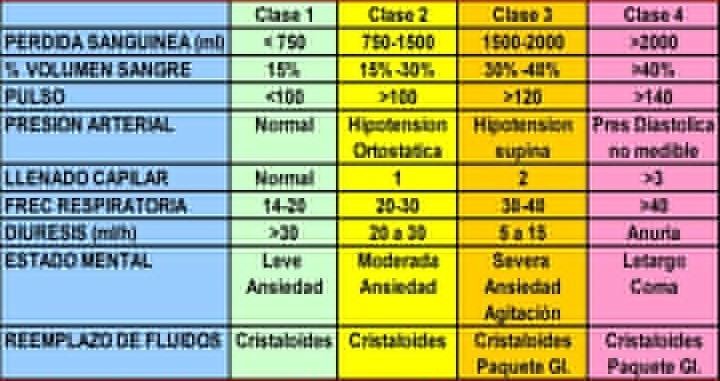
Figure C 6. Hemodynamic parameters
of hypovolemic shock

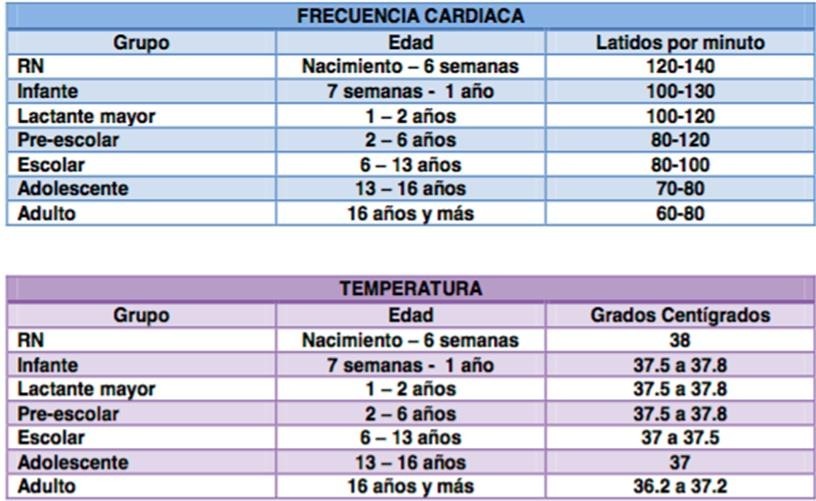
Figure C 7. Table of normal values
of vital functions
Appendix
D. Care plan according to AREA model
AREA
Model
(Modified)
FRAMEWORK
Professional
Reflection: After having provided adequate nursing
care during the patient's stay in the obstetrics and gynecology hospital, the
patient has been able to control the episode of threatened abortion, as shown
by the comparison of the initial values of the indicators with the assessment
of the same in periods of time from 6 to 24 hours, confirmed by the favorable
evolution without risk of losing her pregnancy for the time being.
Person
EVALUATION:
Patient
22 years old, admitted for emergency in wheelchair, accompanied by family
member, was evaluated by the doctor and Dx. of threatened abortion, with
gestation of 11 weeks by ultrasound, amenorrhea more than two years (by use of
hormonal contraceptive method injectable every 3 months), first pregnancy
(euthyroid delivery and term), abdominal ultrasound. She denies previous
abortion and denies allergies.
Hemoglobin
of 10.5 mg/dl, Subunit (beta-hCG) of 13800, three doses of tetanus vaccine in
her first pregnancy.
(00221)
Ineffective
maternity process
r/c
with
inadequate prenatal care, inadequate maternal nutrition m/p
inadequate
prenatal management, ineffective management of bothersome symptoms during
pregnancy and inadequate prenatal lifestyle.
Person
Dx. NURSING
PLAN
OF CARE
NOCp
Indicator
(1607) Prenatal health behavior
Indicator
(160703) Maintains pre-birth attendance visits
Indicator
(160710) Maintains adequate nutrient intake for gestation.
Indicator
(160723) Uses iron supplementation
Indicator
(160714) Prevents exposure to infectious diseases.
Indicator
(160721) Uses medicines according to prescription
State/Behavior/
Perception
Weakness
Inamobility Insomnia
Start
of prenatal care
Patient
with hemoglobin of 10.5 mg/dl
Patient
with hemoglobin of 10.5 mg/dl
Dark
brown vaginal discharge.
Prescription
medication
Standard
of normality
Counseling:
maternal and fetal care during pregnancy. As well as warning signs
Recommendations:
start prenatal care after discharge from the hospital
Recommendations
for consumption of an iron-rich diet
Progressive
increase of hemoglobin with treatment.
Absence
of vaginal discharge
Full
treatment compliance
Indicator
(1607) Sanitary behavior
Indicator
(160703) Maintains visits from pre natal care
Indicator
(160710) Maintains an intake of nutrients suitable for gestation.
Indicator
(160723) Uses iron supplements
Indicator
(160714) Avoid exposure to diseases infectious diseases.
Indicator
(160721) Uses medicines according to subscription
With
the nursing care administered to the patient being
With
the 24-hour nursing care administered to the patient be it achieved a Dartboard
score of 5 (+4)
With
the 24-hour nursing care administered to the patient be it achieved a Dartboard
score of 5 (+3)
With
the 24-hour nursing care administered to the patient be it achieved a Dartboard
score of 5 (+4)
With
the 26 hours of nursing care administered to the patient be it achieved a
Dartboard score of 4 (+2)
With
the 24-hour nursing care administered to the patient be it achieved a Dartboard
score of 5 (+4)
Likert
scale: 1-Never demonstrated. 2-Rarely demonstrated. 3-Sometimes demonstrated.
4-Frequently demonstrated. 5-Always demonstrated.
NICs
for NOCs (DxEp) (6680) Vital signs monitoring
(Butcher et al., 2019, p. 341) Activities:
(668001)
Monitor blood pressure, pulse, temperature and respiratory status.
(668002)
Observe blood pressure trends and fluctuations.
(668003)
Monitor respiratory rate and rhythm (depth and symmetry).
(668004)
Monitor pulse oximetry.
(668005)
Periodically monitor skin color, temperature and moisture.
(4150)
Hemodynamic regulation (Butcher et al., 2019, p. 393).
Activities:
(415001)
Perform a thorough assessment of hemodynamic status (check blood pressure,
heart rate, pulses, venous pressure).
(415002)
Recognize the presence of early warning signs and symptoms indicative of system
compromise.
hemodynamic.
(415003)
Determine perfusion status (indicate whether the patient is cold, warm or hot)
(415004) Monitor inflow and outflow, diuresis and patient's weight
(1450)
Nausea management (Butcher et al., 2019, p. 296)
Activities:
(145001)
Monitor antiemetic treatment effectiveness
(145002)
Encourage patient to self-manage nausea
(145003)
Promote adequate rest/sleep to alleviate nausea
(145004)
Recommend small, appealing meals
(145005)
Weigh patient regularly
Likert
scale: 1-Never demonstrated. 2-Rarely demonstrated. 3-Sometimes demonstrated.
4-Frequently demonstrated. 5-Always demonstrated.
NICs
for NOCs (RCp)
(4410)
Hemorrhage prevention
Activities:
(441001)
Closely monitor for signs of internal/external bleeding (e.g., abdominal
swelling)
(441002)
Record Hb/Hct levels pre- and post-bleeding
(441003)
Maintain IV access
(441004)
Enforce bed rest during active bleeding
(441005)
Educate patient/family on bleeding signs
(5310)
Hope instillation
Activities:
(531001)
Help patient/family identify hopeful aspects
(531002)
Foster therapeutic relationships with loved ones
(531003)
Assist in setting/reviewing hope-related goals
(531004)
Facilitate religious practice if applicable
(531005)
Avoid masking the truth
(5270)
Emotional support
Activities:
(527001)
Explore emotional triggers
(527002)
Support healthy coping mechanisms
(527003)
Encourage talking/crying to reduce distress
(527004)
Provide reassurance during anxiety peaks
(527005)
Refer to counseling if needed
Appendix
E. Care plan according to the BIFOCAL model
BIFOCAL
Model
(Modified)
Person
VALUATION:
Patient
22 years old,
Person
RC
p
RC
HEMORRHAGE
FRAME
Professional
Reflection: NOC DxEp - Gestation in its first 20
weeks is at risk of threatened abortion (spontaneous or induced), causing signs
similar to other pathologies that require discarding, hence the importance of
pre-natal control to prepare for a viable pregnancy. Every threatened
miscarriage is accompanied by physical and spiritual suffering, as well as
other signs that suggest pregnancy loss such as pain and vaginal bleeding was
admitted in an emergency wheelchair, accompanied by a family member, was
evaluated by the doctor and diagnosed with threatened abortion, with an 11-week
gestation by ultrasound, amenorrhea for more than two years (due to the use of
hormonal contraceptive injectable every 3 months).
Planning
NOCp (DxEp) (1607) Prenatal health behavior
Indicator
(160703) Maintains pre-birth attendance visits
Indicator
(160710) Maintains adequate nutrient intake for gestation.
Indicator
(160723) Use iron supplements
Indicator
(160714) Prevents exposure to infectious diseases.
Indicator
(160721) Uses medicines according to prescription
With
the nursing care administered to the patient, a target score of 5 (+4) was
achieved.
With
the nursing care administered to the patient, a target score of 5 (+3) was
achieved.
With
the nursing care administered to the patient, a target score of 5 (+4) was
achieved.
With
the nursing care administered to the patient, a target score of 4 (+3) was
achieved.
With
the nursing care administered to the patient, a target score of 5 (+4) was
achieved.
(RCp)
(0413) PI
(041307)
Bleeding vaginal
(041313)
Pallor of skin and mucous membranes
(041306)
Strain abdominal
(041316)
Decrease in the Hb.
(041317)
Decrease of hto
(041314)
Anxiety
(041309)
Systolic BP decrease
(041309)
PA decrease diastolic
(041309)
Loss of body heat
With
the nursing care provided, a Diana score of 5 (+1) was achieved.
With
the nursing care provided, a Diana score of 5 (+2) was achieved.
With
the nursing care provided, a Diana score of 5 (+2) was achieved.
With
the nursing care provided, a Diana score of 5 (+2) was achieved.
With
the nursing care provided, a Diana score of 5 (+2) was achieved.
achieved
a Diana score of 5, (+1)
With
the nursing care provided, a Diana score of 5 (+1) was achieved.
pregnancy
(euthyroid delivery at term), abdominal ultrasound. She denies previous
abortion and denies allergies.
Hemoglobin
10,5
mg/dl, Subunit
(beta-hCG) of 13800. Three doses of tetanus vaccine in her first pregnancy.
Likert
scale: 1-Never demonstrated. 2-Rarely demonstrated. 3-Sometimes demonstrated.
4-Frequently
demonstrated 5-Always demonstrated.
NICs
for NOCs (DxEp)
(6680)
Vital signs monitoring. (Butcher et al., 2019, p. 341)
Activities:
(668001)
Monitor blood pressure, pulse, temperature and respiratory status.
(668002)
Observe blood pressure trends and fluctuations.
(668003)
Monitor respiratory rate and rhythm (depth and symmetry).
(668004)
Monitor pulse oximetry.
(668005)
Periodically monitor skin color, temperature and moisture.
(4150)
Hemodynamic regulation (Butcher et al., 2019, p. 393).
Activities:
(415001)
Perform a thorough assessment of hemodynamic status (check blood pressure,
heart
rate, pulses, venous pressure).
(415002)
Recognize the presence of early warning signs and symptoms indicative of a
compromise
of
the hemodynamic system.
(415003)
Determine perfusion status (indicate whether the patient is cold, warm or hot)
(415004) Monitor inflow and outflow, diuresis and patient's weight
(1450)
Management of nausea (Butcher et al., 2019, p. 296).
Activities:
(145001)
Monitor the effect of treatment of nausea.
(145002)
Encourage the patient to control her own experience of nausea. (145003)
Encourage adequate rest and sleep to facilitate relief of nausea.
(145004)
Encourage ingestion of small amounts of food that is appealing to the nauseated
person.
(145005)
Weigh the patient regularly.
Likert
Scales: 1-Severe. 2-Substantial. 3-Moderate. 4-Leve. 5-None.
NICs
for NOCs (RCp)
(4410)
Prevention of hemorrhage.
Activities:
(441001)
Monitor patient closely for signs and symptoms of internal or external
bleeding.
(example:
abdominal swelling).
(441002)
Record hemoglobin and hematocrit levels before and after blood loss,
as
indicated.
(441003)
Maintain intravenous access.
(441004)
Maintain bed rest during active bleeding. (441005) Instruct patient and/or
family on signs of bleeding.
(5310)
Give hope.
Activities:
(145001)
To help the patient and family identify areas of hope in life.
(145002)
Foster therapeutic relationships with loved ones.
(145003)
Help the patient design and review goals related to the object of hope.
(145004) Create an environment that facilitates the patient's practice of her
religion, when possible. (145005) Avoid disguising the truth.
(5270)
Emotional Support.
Activities:
(527001)
Explore with the patient what triggered the emotions.
(527002)
Support the use of appropriate defense mechanisms.
(527003)
Encourage conversation or crying as a means of decreasing the emotional
response. (527004) Stay with the patient and provide feelings of security
during periods of heightened anxiety.
(527005)
Refer to counseling services if needed.
![]() *
*![]()