doi: 10.62486/agmu202499
REPORT CASE
Usefulness of ultrasound in the diagnosis of lumbricoid ascaris. Case Report and Literature Review
Utilidad de ecografía en el diagnóstico de Áscaris Lumbricoides. Reporte de Caso y Revisión de la Literatura
Ismael Vargas Gallego1
 *,
Jhossmar Cristians Auza-Santivañez2
*,
Jhossmar Cristians Auza-Santivañez2
 *,
Ariel Sosa Remón3
*,
Ariel Sosa Remón3
 *,
Eloy Paycho Anagua4
*,
Eloy Paycho Anagua4  *,
Marco Antonio Gumucio Villarroel4
*,
Marco Antonio Gumucio Villarroel4
 *,
Ritdber Alfredo Quispe Sarmiento5
*,
Ritdber Alfredo Quispe Sarmiento5
 *,
Mildred Ericka Kubatz La Madrid6
*,
Mildred Ericka Kubatz La Madrid6
 *
*
1Hospital de Tercer Nivel Dr. Hernán Messuti Ribera. Pando, Bolivia.
2Ministerio de Salud y Deportes. Instituto Académico Científico Quispe-Cornejo. La Paz, Bolivia.
3Instituto Nacional de Oncología y Radiobiología. Habana, Cuba.
4Hospital de Tercer Nivel Dr. Hernán Messuti Ribera. Pando, Bolivia.
5Hospital de Tercer Nivel Daniel Bracamonte. Potosí, Bolivia.
6Hospital Boliviano Japonés «Dr. Roberto Galindo Terán». Pando, Bolivia.
Cite as: Vargas Gallego I, Auza-Santivañez JC, Sosa Remón A, Paycho Anagua E, Gumucio Villarroel MA, Quispe Sarmiento RA, et al. Usefulness of ultrasound in the diagnosis of lumbricoid ascaris. Case Report and Literature Review. Multidisciplinar (Montevideo). 2024; 2:99. https://doi.org/10.62486/agmu202499
Submitted: 21-12-2023 Revised: 06-04-2024 Accepted: 05-08-2024 Published: 06-08-2024
Editor: Telmo
Raúl Aveiro-Róbalo ![]()
Autor para la correspondencia: Jhossmar Cristians Auza-Santivañez2 *
ABSTRACT
Introduction: the World Health Organization (WHO) points out that more than a third of the world’s population is infected by one or more parasites. Ascariasis is the most prevalent parasitic disease in the world, with approximately 664 million people infested.
Clinical case: a 22-year-old female patient enters the emergency department with general malaise, with worsening symptoms in recent days, intense abdominal pain, associated with nausea and uncontrollable vomiting. She also reports non-elimination of gas and absence of bowel movements. An emergency ultrasound is requested, it reports the stomach with the presence of a linear, tubular echogenic image that moves in different directions.
Discussion: the widespread use of ultrasound in Emergency Departments for the diagnosis of acute abdomen, as well as in the laboratory, allowed us to reach the presumptive diagnosis of temporary biliary obstruction due to A. lumbricoides, in addition, the presence of jaundice, direct hyperbilirubinemia and discrete elevation gamma-glutamyltransferase (GGT); findings that could direct the exploration of the bile duct during the surgical procedure.
Conclusions: the importance of the clinical case lies in the use of abdominal ultrasound as a diagnostic method for Ascaris Lumbricoides. The use of ultrasound in emergency services is essential in the presence of an acute abdomen, and in any patient who presents acute biliary symptoms, always think about this pathology.
Keywords: Ascaris Lumbricoides; Biliary Obstruction; Jaundice; Ascariasis.
RESUMEN
Introducción: la Organización Mundial de la Salud (OMS) señala que más de la tercera parte de la población
mundial está infectada por uno o más parásitos. La ascaridiasis es la parasitosis de mayor prevalencia en el mundo, con aproximadamente 664 millones de personas infestadas.
Caso clínico: paciente femenina de 22 años de edad, ingresa al servicio de emergencias con un cuadro malestar general, con empeoramiento de los síntomas en los últimos días, dolor abdominal intenso, asociado a náuseas y vómitos incoercibles, además refiere no eliminación de gases y ausencia de deposiciones. Se solicita una ecografía, de emergencia, la misma informa estomago con presencia de imágen ecogénica lineal, tubular que se mueve en diferentes direcciones.
Discusión: el extendido uso de la ecografía en los servicios de Urgencias para el diagnóstico del abdomen agudo, así como el de laboratorio, permitió llegar al diagnóstico presuntivo de obstrucción biliar temporal por A. lumbricoides, además, la presencia de ictericia, hiperbilirrubinemia directa y discreta elevación de la gama-glutamiltransferasa (GGT); hallazgos que pudieron direccionar a la exploración de la vía biliar durante el acto quirúrgico.
Conclusiones: la importancia del caso clínico radica en el uso de la ecografía abdominal como método de diagnóstico del Ascaris Lumbricoides. Se hace indispensable el uso de la ecografía en los servicios de urgencias ante la presencia de un abdomen agudo, además en todo paciente que presente síntomas biliares agudos, pensar siempre en esta patología.
Palabras clave: Ascaris Lumbricoides; Obstrucción Biliar; Ictericia; Ascaridiasis.
INTRODUCTION
The World Health Organization (WHO) reports that more than one-third of the world's population is infected with one or more parasites and that approximately 155 000 people die each year from complications associated with this disease. Ascariasis is the most prevalent parasitic disease in the world, with approximately 664 million people infected.(1,2,3) It is also prevalent in the pediatric population, a situation favored by the displacement of infected people, combined with economic and environmental factors, and poor hygiene conditions. Parasitic diseases are currently a public health problem. The impact of this disease in Bolivia is not clearly defined. However, communities still live in unfavorable economic, cultural, and environmental conditions. In its different modalities, abdominal ultrasound is a pillar in diagnosing many entities, especially in identifying signs such as the "worm mass" and "double tube."
Ascaris lumbricoides is known as the roundworm. It was first described in 1758 by the Swedish zoologist Carl Linnaeus.(4) It has been known since ancient times; the Greeks called it Elnus strongyle. Hippocrates mentions it as a parasite of infants, and the Romans called it Lumbricus teres, as they could not distinguish it from earthworms. In Korean mummies from the Joseon kingdom in the 15th century, A. lumbricoides eggs were found in good condition. Despite being known since ancient times, it was not until 1916 that Stewart demonstrated the pulmonary cycle of the parasitic disease in experiments on rodents. Subsequently, in 1922, the Koino brothers confirmed the life cycle in humans through self-infection and the presence of larvae in sputum. There is evidence of the disease since ancient times. Mummies from ancient Egypt infected with this parasite have been found, as well as Ascaris lumbricoides eggs in human coprolites in Peru dating back to approximately 2277 BC. Given the large size of this worm, its existence must have been quite obvious, and many ancient writings refer to this infection. The Ebers Papyrus, from the 15th century BC, mentions its existence and treatment, and Hippocrates, Chinese, Arab, and Roman doctors all wrote about it at the time. By 1915, Stewart described the life cycle of the helminth, including its passage through the lungs, and in 1922, Koino in Japan experimentally ingested 2 000 Ascaris lumbricoides eggs. Eleven days later, he found larvae in his sputum, and days later, he eliminated 667 worms through his stool after administering an antihelminthic, establishing the complete cycle.(5)
Ascariasis is more prevalent in children in tropical and developing countries, where soil contamination by human feces and the use of untreated feces as fertilizer perpetuate it. Ascaris lumbricoides are elongated, cylindrical worms with bilateral symmetry, unsegmented, and with separate sexes. They are transmitted via the digestive tract, fecal-oral.(6)
Among the countries with the highest incidence of geohelminthiasis are Brazil, Colombia, Mexico, Bolivia, Guatemala, Haiti, Honduras, Nicaragua, Peru, and the Dominican Republic.(7) In Bolivia, it is known to be the most prevalent, with studies conducted in the highlands attributing a prevalence of 1,4 %, in the valleys from 5,0 % to 83,0 %, and tropical areas from 15,0 % to 96 %.(8)
CLINICAL CASE
A 22-year-old female patient was admitted to the emergency department of the Japanese Hospital "Dr. Roberto Galindo Teran" with general malaise, symptoms of coldness and pale skin, sweating, and a history of abdominal pain, weakness, occasional dry cough, and loss of appetite for three months, with worsening symptoms in the last few days, severe abdominal pain associated with nausea and uncontrollable vomiting, as well as an inability to pass gas and no bowel movements.
Physical examination was very acute, with tachycardia and blood pressure of 60/30 mmHg. Auscultation revealed arrhythmic heart sounds. Abdomen: decreased bowel sounds, soft abdominal wall, depressed and painful on palpation. No visceromegaly.
The surgery department evaluated him. They suspected intestinal obstruction and requested an emergency ultrasound. The ultrasound revealed a gallbladder with 8 mm perivascular edema, a stomach with a linear, tubular (mobile) echogenic image in different directions, and a small amount of free fluid (echolucent) in the abdominal cavity. A hypoechoic tubular structure with well-defined echogenic walls could correspond to a parasite (adult worm).
During the real-time evaluation, adult Ascaris worms can be seen curving in the stomach. When the stomach is full of fluid, the Ascaris lumbricoides appears as an echogenic, linear image with linear movement, known as the internal tube sign. Another finding is the spaghetti sign, which is when there is a longitudinal overlap of parasites in the bile duct due to the coiling of one or more Ascaris. The streak sign is a thin streak without an internal tube. The bull's eye sign implies coiling of the parasite. Its motility can be observed on real-time ultrasound. (figure 1A - 1B).
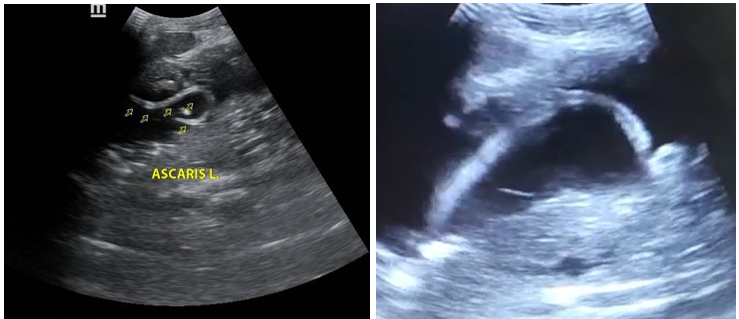
Figure 1. A: Gray scale ultrasound, sagittal section, showing a linear, tubular echogenic image, bull's eye sign. B: Ultrasound shows the sign of the line, which is a thin line without an internal tube and without acoustic shadowing
The abdominal ultrasound was repeated upon the patient's discharge and was normal, as the previously reported images had disappeared.
DISCUSSION
The highest incidence of ascariasis is reported between the ages of 2 and 10, declining significantly after age 15. Similarly, complications due to this parasite also predominate in childhood, due to the small size of their organs and the size that an adult specimen can reach.(9,10) Intestinal or biliary obstruction, cholangiohepatitis, liver abscess, pancreatitis, acute appendicitis, and intestinal perforation are complications that occur due to the large number of specimens and their intraluminal migration.
Initially, obstruction by A. lumbricoides tangles was not considered in the differential diagnosis, probably because the patient was treated in a hospital located in a non-endemic area. However, if we analyze the data retrospectively, such as the patient's origin, the absence of previous pathologies, the subacute presentation of the clinical picture, and the nonspecificity of the laboratory tests, this diagnosis could be considered.
Our patient's diagnosis was based on clinical manifestations and abdominal ultrasound findings. Abdominal ultrasound (with bowel preparation) is recommended when there is suspicion of invasion of the hepatobiliary tract or when searching for parasites in the stool, which, in similar circumstances, has prevented surgery in older adults with good results.(11) Treatment for A. lumbricoides is medical, and surgical management should be expectant due to the high intra- and postoperative morbidity, as occurred in our patient, who, in addition to requiring critical care and monitoring in the ICU, presented with severe hospital-acquired infections.(10)
If medical management fails, emergency surgery is the main indication. According to Sónmez and Hershkovitz, the surgical technique will depend on intraoperative findings, describing the performance of various procedures ranging from intestinal resection, in the event of evidence of gangrene or intestinal infarction, to enterostomy, when perforation is found, or enterotomy if the intestine is intact and only the worms are to be removed. Care must always be taken not to release adult worms or eggs into the abdominal cavity.(10,11)
In our patient, the diagnosis was made before surgery, and the patient's age led us to decide not to prolong the surgical procedure and to choose appropriate medical management. The current availability of endoscopy as a therapeutic tool should be considered. Pekery et al. reported the case of a 78-year-old patient with intestinal obstruction due to A. lumbricoides, in whom they managed to extract multiple adult worms using this technique, followed by treatment with mebendazole, with good results.(12)
Abdominal ultrasound is the method of choice for the diagnosis of biliary ascaris. Findings will depend on the number of ascaris, their location, and the longitudinal or transverse visualization of the parasite. (13) Finally, we consider that our case had a presumed temporary biliary obstruction caused by A. lumbricoides, due to the presence of jaundice, direct hyperbilirubinemia, and a slight elevation of gamma-glutamyltransferase (GGT); findings that led to the exploration of the bile duct during surgery.
Complications of Ascaris Lumbricoides
Growth retardation. Loss of appetite and poor absorption of digested food put children with ascariasis at risk of malnutrition, which can delay growth. Obstruction of ducts. In some cases, worms can block the narrow ducts of the liver or pancreas, causing severe pain. Pneumonia. This corresponds to the transpulmonary migration of the helminth during its life cycle, Ascaris. Pulmonary manifestations occur 5-26 days after ingestion of viable eggs. Ascaris pneumonia can develop from migratory, transient, and localized intra-alveolar inflammatory reactions. Biliary Peritonitis. Due to perforation of the duct. Cholangitis. Due to obstruction of the bile duct. Acute cholecystitis. Due to obstruction of the extrahepatic bile duct or cystic duct, the invasion of the bile duct can cause complications. Obstructive jaundice syndrome. This is caused by obstruction of the bile duct by Ascaris lumbricoides.(13) Acute appendicitis. This is caused by obstruction of the parasite, and the pathophysiology of appendicitis is attributed to a granulomatous reaction in response to the parasite's eggs.(14,15) Intestinal obstruction. In certain patients, especially children, intestinal infestation with adult Ascaris lumbricoides can be so intense due to multiple parasites that they become entangled and can cause a syndrome of subocclusion or definitive intestinal obstruction. Both conditions are characterized by abdominal distension, absence of bowel movements, vomiting, and meteorism. An abdominal mass, which is the "ascaris ball, can be felt." However, intussusception and volvulus may also occur.(14,16) Intestinal perforation. Migration of adults through intestinal openings due to previous surgery, peritoneal granulomas due to egg deposits, and acute appendicitis.(17, 18) Liver abscess. This is caused by the parasite's death, which necrotizes the liver parenchyma tissue, or by obstruction of the bile duct. Liver abscess caused by ascaris is a rare form of presentation.(19,20) Peritonitis. Due to perforation of the intestinal loops or complications of acute appendicitis.(19,20) Acute pancreatitis. Caused by the passage of Ascaris into the pancreatic duct, which can also cause the formation of pseudocysts. Dehydration. Due to fever, prolonged diarrhea, and free fluid in the abdominal cavity.(20) Malnutrition. One of these mechanisms is the inflammatory response generated by parasites. The inflammatory response produces cytokines that cause loss of appetite and deleterious effects on protein metabolism, making its utilization by the body inefficient. Another mechanism is the poor absorption of nutrients in the intestine, mainly due to two situations. The first is utilization by parasites. Calculations indicate that A. lumbricoides can consume up to 100 mg of protein. At the same time, the second mechanism is caused by inflammation of the intestine's inner wall, which increases intestinal transit speed and reduces the time available for proteins to be utilized appropriately. All of this leads to growth retardation and even intellectual development delays. These children are known as "pot-bellied children." Currently, with the development of new ultrasound equipment and innovative techniques, the use of ultrasound of the digestive tract or intestinal ultrasound for diagnostic imaging stands out in inflammatory bowel disease, acute abdomen in adults and children, infectious and tumor pathology of the intestine and peritoneum, and intestinal ultrasound in pediatrics, with highly sensitive and specific results. As presented in the digestive tract ultrasound series by the Spanish Society of Radiology, according to T. Ripollés Gonzales.(21)
CONCLUSIONS
Our clinical case's importance lies in using abdominal ultrasound as a diagnostic method for Ascaris Lumbricoides. The use of ultrasound is essential in emergency departments in the presence of an acute abdomen, and in all patients presenting with acute biliary symptoms, this pathology should always be considered.
REFERENCES
1. Acuña A, Calegari L, Curto S, Lindner C, Rosa R, Salvatella R, et al. Helmintiasis intestinales: manejo de las Geohelmintiasis. Montevideo: OPS, 2008.
2. Organización Panamericana de la Salud. Marco de referencia de un programa regional para el control de las geohelmintiasis y esquistosomiasis en América. Santo Domingo: OPS, 2003:5-35.
3. Arcia M, Carrillo N, Quintero G, Oliva G. Ascariasis biliar. Rev Venez Cir 1990; 43(1):33-5.
4. Pearson R, 2017. Ascariasis. Obtenido de: https://www.msdmanuals.com/es-
5. Bethony J, Brooker S, Albonico M, Geiger SM, Loukas A, Diemert D, et al. Soiltransmitted helminth infections: Ascariasis, trichuriasis, and hookworm. Lancet.2006;367:1521–32.
6. Walker M, Hall A, Basánez˜ MG. Individual predisposition, household clustering and risk factors for human infection with Ascaris lumbricoides: New epidemiological insights. PLoS Negl Trop Dis. 2011;5:e1047.
7. OPS/OMS | Organización Panamericana de la Salud. Geohelmintiasis [Internet]. Geohelmintiasis en las Américas para público en general. 2017 [citado 3 de diciembre de 2021]. Disponible en: https://www.paho.org/es/temas/geohelmintiasis.
8. Sergio Mollinedo, Cecilia prieto. El enteroparasitismo en Bolivia. 2006.
9. C. Hommeyer, G. S. Hamill, J. A. Johnson. CT diagnosis of intestinal ascariasis. Abdom Imaging 20:315 -316 (1995)
10. Eric J. Rodriguez, MD, Maggie A. Gama, MD, Sanford M. Ornstein, MD, William D. Anderson, MD. 2003. Ascariasis Causing Small Bowel Volvulus. RadioGraphics 2003, 23:1291-1293.
11. CJ Das, J Kumar, J Debnath, A Chaudhry. Imaging of ascariasis. Australasian Radiology (2007) 51, 500-506. https://doi.org/10.1111/j.1440-1673.2007.01887.x
12. Q.F. Angela Del Rocio Mite Parrales. “Incidencia de parasitismo por ascaris lumbricoides en la parroquia Manuel j. calle”. 2001.
13. Castaño, R., Yepes, N.L., Sanín, E., &Sepúlveda, M. (2013). Ascaridiasis biliar: manejo endoscópico. Rev Colomb Gastroenterol.,18, 83-87.
14.
Coello, L. (2012). Repercusión sobre la Productividad Estudiantil de las
Helmintiasis Intestinales. Revista Médica de Nuestros Hospitales, 18 (4), 183-
186. Recuperado de
https://www.revistamedica.org.ec/vol18no4/2441-repercusion-sobre-la-productividadestudiantil-de-las-helmintiasis-intestinales.
15. Napoleón González Saldañaa, Javier Ordoñez Ortegaa, Cecilia Ridaura-Sanzb, Salim Kuri Ayalac, José Iván Castillo Bejarano. Arch. Pediatr. Urug. complicaciones simultáneas de ascariasis invasiva: migración errática. 2019
16. Alfredo Chiappe, Kovy Arteaga, Cristhian Resurrección, Marcos Ñavincopa y Eduardo Ticona. Obstrucción intestinal por Ascaris lumbricoides en un adulto mayor. 16 de agosto de 2016.
17. Chiappe, A., Arteaga, K., Resurrección, C., Ñavincopa, M., & Ticona, E. (2016). Obstrucción intestinal por Ascaris lumbricoides en un adulto mayor. Revista chilena de infectología, 33(5), 572-575. https://dx.doi.org/10.4067/S0716-10182016000500014.
18.
Neira, J., Manzo, C., Abad, L., & Santana, R. (2018). Isquemia intestinal
por vólvulo de intestino delgado ocasionado por Ascaris
múltiple. A propósito de un caso. Revista Médica de Nuestros Hospitales, 18
(4),187-190. Recuperado de
https://www.juntadebeneficencia.org.ec/revista/vol18no4/2442-isquemia-intestinal.
19. Orellana, A., Gonzabay, M., & Mosquera, R. (2010). Complicaciones hepatobiliares: Ascaridiasis y litiasis coledociana. Revista Médica de Nuestros Hospitales, 16 (1), 28-31. Recuperado de https://www.juntadebeneficencia.org.ec/revista/numeros-anteriores/513-revistamedica-vol16-no1.
20. Tuñón Pitalua, M., Martínez Muñoz, E., & Gómez Villa, J. (2014). Ascariasis hepática. Reporte de un caso y revisión de la literatura. Salud Unmite Barranquilla (Col). 30(2):252-257. Recuperado de http://www.scielo.org.co/pdf/sun/v30n2/v30n2a16.pdf.
21. T. Ripollés González. Radiología. (2020). Presentacion de la serie ‘ecografía del tracto digestivo’. Rev., de la Sociedad Española de Radiologia (SERAM), 62(6):500-501. Recuperdado de https://doi.org/10.1016/j.rx.2020.04.002
CONSENT
The patient's consent was obtained for the performance of this work.
FINANCING
The authors did not receive funding for the implementation of this study.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHOR CONTRIBUTION
Conceptualization: Ismael Vargas Gallego.
Research: Jhossmar Cristians Auza-Santivañez, Ismael Vargas Gallego.
Methodology: Jhossmar Cristians Auza-Santivañez, Ariel Sosa Remón.
Visualization: Ariel Sosa Remón, Marco Antonio Gumucio Villarroel.
Original draft: Ismael Vargas Gallego, Jhossmar Cristians Auza-Santivañez, Eloy Paycho Anagua, Marco Antonio Gumucio Villarroel, Ritdber Alfredo Quispe Sarmiento, Ariel Sosa Remón, Mildred Ericka Kubatz La Madrid.
Writing-revision and editing: Ismael Vargas Gallego, Jhossmar Cristians Auza-Santivañez, Eloy Paycho Anagua, Marco Antonio Gumucio Villarroel, Ritdber Alfredo Quispe Sarmiento, Ariel Sosa Remón, Mildred Ericka Kubatz La Madrid.